Introduction
Clinical research starts with medical practice. There is evidence that ancient Egyptian, Greek, and Chinese physicians conducted clinical studies, including studies of drugs, surgery, and devices.1) Hundreds of studies related to hearing have been conducted in the USA. In Korea, over 100 studies related to hearing or otology are published annually in national or international journals. Clinical research is not limited to universities or tertiary hospitals. Most otologists and audiologists know that Institutional Review Board (IRB) permission is essential when conducting clinical trials involving humans. Many ethical issues arise in clinical practice and clinical research. As physicians and researchers, we often care for patients and conduct clinical research simultaneously.2) However, conflict between clinical practice and research can arise. For example, a research participant may not gain any benefit from the research, but the research may have great benefit for others. When one finds a potentially good drug or treatment for a disease, one wants to test it. Therefore, one must know bioethics and IRB principles and regulations so as to get IRB approval to conduct clinical research. As with clinical guidelines and well-known treatment protocols, there are rules that must be followed. Additionally, governments may restrict clinical trials by law (Table 1).
History of Clinical Research and Bioethics
Clinical trials started with the beginning of medicine. Perhaps ethical issues were also a part of medicine at that time. The first chapter of Daniel in the Old Testament (Daniel 1: 11-16) contains evidence of a clinical trial, and Hippocrates tried to define ethical issues in medicine. However, ethical issues emerged as a major concern in clinical trials before World War II. As a result of Nazi experiments and other unethical experiments conducted in the 20th century, codes and regulations have been drawn up to protect human subjects (Table 1).3-8) The judgment at Nuremberg with respect to the Nazi experiments identified two essential ethical points: voluntary consent and the rights or welfare of the subject (Table 2).1,3)
The Declaration of Helsinki, originally issued by the World Medical Assembly in 1964, has been revised seven times as of 2011.6,9) The guiding principle is "the health of my patient will be my first consideration". Although the declaration applies primarily to physicians, the World Medical Assembly encouraged those conducting related medical research to follow their principles. They defined several requirements for the scientific and ethical aspects of research to be applied by physicians, authors, and ethics committees.6)
Principles of Bioethics
There are several principles in bioethics. The three basic principles identified in the Belmont report in 1979 were respect for persons, beneficence, and justice. These principles are manifested in informed consent, the assessment of risk and benefits, and the selection of subjects.10)
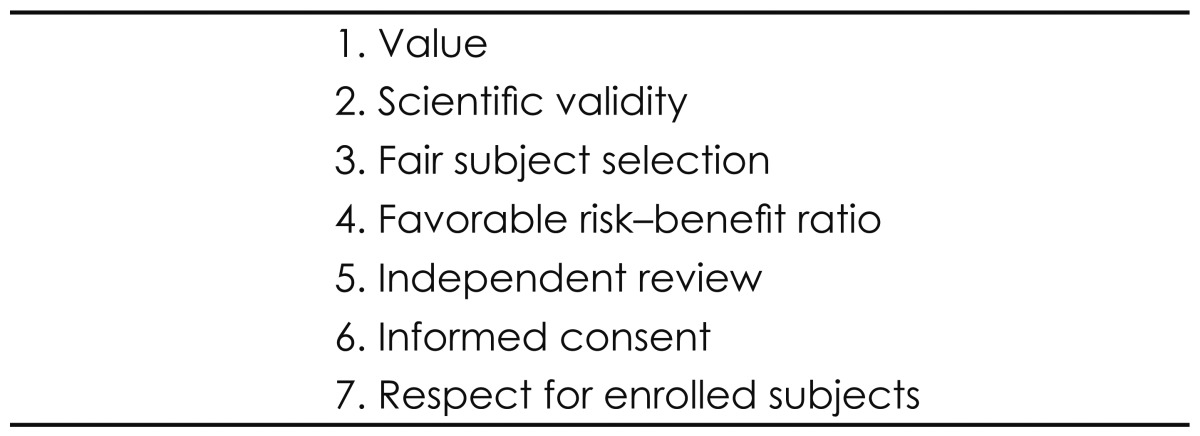
The seven ethical requirements published in the Journal of the American Medical Association in 2000 are also well-known and well-organized principles (Table 3).11) Fulfillment of all seven requirements is necessary for ethical clinical research.11,12) These requirements are universal, but they must be adapted to the health, economic, cultural, and technological conditions under which clinical research is conducted.
Clinical trials are valuable if the clinical research improves health and well-being or advances knowledge. To be ethical, clinical research must be valuable. All clinical research exploits patients and uses limited resources. So investigators should consider the value of any clinical trial.13)
Scientific validity means that the researcher should use accepted scientific principles and methods, including statistical methods, to produce reliable, valid data.4) In clinical research, a scientific study may be an ethical study; an unscientific study is an unethical study. Subject selection must be fair so that stigmatized or vulnerable subjects are not targeted for risky research. A scientific study requires fair subject selection using scientifically valid selection and exclusion criteria. Through this process, the investigator can manage risks and benefits, such as excluding higher-risk groups.14,15)
Clinical trials can be conducted only if they have a favorable risk-benefit ratio.16) Risk is the probability of harm or injury caused by the clinical trial. Minimal risk is defined as "the probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance of routine physical or psychological examinations or tests" [Code of Federal Regulations (CFR) 45, 46]. Benefit refers to valued or desired outcomes related to health, psychosocial state, or knowledge. Money is not a benefit, but can be considered as compensation.17) The assessment of risk and benefits involves three steps. First, risks are identified and minimized. Risk can be reduced by using a scientific study design and reducing unnecessary exposure to risk.18,19) Second, benefits are increased if the health of the subjects is improved, knowledge about their disease is increased, or a clinical service is provided. Finally, the balance between risks and benefit should be assessed. The cumulative benefit of a clinical trial should outweigh its risk.
Independent review is essential when conducting clinical trials because every investigator has an inherent conflict of interest.20) The independent reviewers should not be affiliated with the research to minimize any conflict of interest.21,22) The independent review includes not only the IRB but also data- and safety-monitoring boards or ethics committees.23) An independent reviewer reviews the design of the research, the proposed subject population, and the risk-benefit ratio of the study. Minimum standards have been defined for IRB membership: the IRB should have at least five members including at least one member with a scientific background, one nonscientific member, and one person who is not affiliated with the institution.5)
The investigator should respect subject autonomy and shou-ld obtain informed consent.24) Informed consent must ensure that individuals control their enrollment in clinical trials and their continuing enrollment. Any informed consent process should include notifying the subject of the purpose of the research as well as its procedures, potential risks, benefits, and alternatives. In the USA, the general requirements for informed consent are regulated by the CFR (Table 4).5)
IRB Review Process
The aim of most IRBs is to protect the rights and welfare of humans participating as subjects in research studies. The IRB approves and monitors clinical trials. Although the IRB review process varies according to region and institution, it includes common steps and rules.13,25) The process starts with the submission of a research proposal. The proposal usually includes the application form, study protocol, case report form, curriculum vitae of the investigators, and statement of conflicts of interest. Additionally, most IRBs require the completion of good clinical practice training, Collaborative Institutional Training Initiative training, or other training to ensure that the investigators are prepared to conduct ethical research.
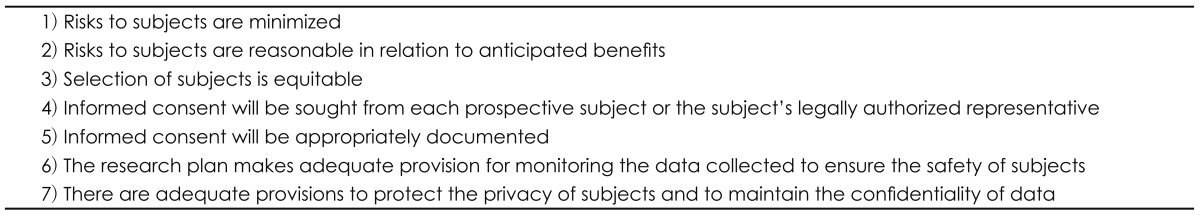
When the proposal is submitted, the IRB reviews it in terms of its scientific and ethical merit.26) In the USA, CFR 46 suggests that regulatory review is a requirement (Table 5).5) After the review, the protocol is voted on; the vote may be open or closed. Four basic outcomes are possible: approval, conditional approval, revision required, and rejection. After obtaining IRB approval, clinicians can start their studies. Typically, the IRB requires that the approval be renewed annually if the study will continue for several years.
Conclusions
Before commencing clinical research, it is important to know bioethics as well as the IRB rules. As otologists and audiologists,
we can reduce the risk to participants and provide more information for informed consent in studies involving hearing-impaired patients. Any well-designed study protocol should meet scientific and ethical guidelines.