|
 |
- Search
| J Audiol Otol > Volume 26(3); 2022 > Article |
|
Abstract
Background and Objectives
The COVID-19 pandemic has led to widespread use of telepractice in hearing health care services. In this study, we investigated the knowledge, attitude, and practice (KAP) of tele-audiology among Indian audiologists. The current study is based on tele-practice guidelines recommended by the Indian Speech and Hearing Association for tele-audiology services in India.
Subjects and Methods
An internet-based KAP questionnaire survey was performed among 108 audiologists. The questionnaire included 33 items categorized under the following domains: demographic information and KAP of tele-audiology. Of the 108 audiologists included in the study, 38 admitted to the practice of tele-audiology previously and during the COVID-19 pandemic (tele-practitioners), and 70 respondents had no experience of tele-audiology (non-telepractitioners).
Results
Overall higher scores were observed with regard to the knowledge domain, and a mixed attitude regarding tele-practice was observed among audiologists. Most respondents acknowledged the advantages of tele-audiology in clinical practice. However, audiologists were hesitant to utilize this technology owing to the challenges associated with tele-practice.
Conclusions
Despite adequate awareness and a positive attitude, a gap is observed between available knowledge and its actual application/utilization in tele-audiology. Tele-audiology practice was limited to counseling, hearing impairment treatment, and troubleshooting tips for hearing aids. Evidence-based practices to perform diagnostic test battery in tele-mode, hands-on training to run diagnostic test battery/rehabilitation using a tele-mode approach, and greater understanding of the technical requirements for tele-practice may result in a positive perception and encourage tele-audiology practice among audiologists. Specialized training and regular continuing education programmes are important to promote tele-audiology services in clinical practice.
The effect of COVID-19 pandemic and nationwide lockdowns have disrupted and minimized the face to face health care consultations. The hearing health care providers/ audiologists were not prepared to face these consequences. Tele-audiology is an emerging option to reach out audiological services in remote areas as well as during COVID-19 pandemic. This mode of service delivery has been utilized in varying capacities such as general consultations, screening, diagnostic assessments, rehabilitation, and counseling [1]. In many countries, tele-audiological services were limited to counseling and online administration of hearing screening questionnaire as only a few proportions of audiologists had the provision and infrastructure to offer tele-audiological services.
Several researches were focused on understanding patients/service seekers opinion and satisfaction with tele-audiological services [1-5]. The success of the implementation of new technology/practice in health care depends not only on the patient satisfaction but also on the satisfaction of the service providers. There are only a few studies that had explored the audiologists’ perceptions on tele-audiology [3,6,7]. Eikelboom and Swanepoel [3] surveyed audiologists from around the world on the use of computer and video-conferencing technology and willingness to use tele-technology to provide audiological services. Majority of the respondents reported that they were comfortable using tablet, computer, and video conferencing software. Though, majority reported of familiarity with tele-audiology and willingness to practice tele-audiology, only 15% of audiologists reported of actually using tele-audiology. Although this survey was across 37 countries, majority of the responses were from South Africa, New Zealand, United States, Australia, and Canada. One of the limitations of this study is it does not reflect the spread of audiologists across the globe.
Singh, et al. [7] surveyed health care practitioner’s attitudes toward tele-audiology appointments and willingness to conduct different clinical tasks on different patient populations. Majority of the respondents indicated that tele-audiology has minimal effect on hearing health care. A small proportion of respondents believed that tele-audiology would have negative impact on quality of care in audiology. The results obtained from this cannot be generalized as the data is the representation of Canadian hearing healthcare practitioners.
Only one study surveyed speech language pathologists and audiologists’ perspectives on tele-services in India [6]. The survey showed that only 12% of the respondents were engaged in tele-practice in India. However, information on infrastructure availability, resource materials requirement, and the challenges faced by the tele-practitioners were not addressed in this study.
Another literature from India was on a systematic review on knowledge and perceptions of tele-audiology among audiologists [8]. The review was based on 5 studies that were carried out in Western countries (USA, Canada, South Africa, New Zealand, and Australia). The uptake of tele-technology varies across the globe due to various factors such as technology advancement, resource constraint/availability, lack of infrastructure or guidelines pertaining to tele-practice. Tele-practice application varies drastically in low-mid income countries, and hence, the study results cannot be generalized to developing countries such as India. All the above reported literature were prior to the COVID pandemic.
Recently, during the pandemic, few studies explored the effect of COVID-19 on audiological services. Saunders and Roughley [9] documented changes in audiology practice during COVID-19 through a survey on 120 audiologists in UK. Around 30% of the audiologists reported of using tele-audiology prior to COVID-19, 90% of the audiologists during the pandemic and 86% of the audiologists reported that they will continue with the tele-practice even when the restrictions are lifted. Though the audiologists expressed positive experience with tele-audiology, majority of them expressed the need of improvements in infrastructure and training in providing tele-audiological services. The results of this study were based on a specific geographical location (UK). Due to COVID pandemic and the upsurge in information technology, there is a change in the healthcare delivery across the globe. Hence, there is a need to study audiologist’s knowledge, attitude, and practice (KAP) towards tele-audiology in the current scenario in India.
A recent survey by Gunjawate, et al. [10] explored the impact of COVID-19 on professional practices of audiologists and speech-language pathologists in India through a KAP survey on 211 audiologists and speech language pathologists. Questions on the knowledge of symptoms of COVID-19 and its preventive measures, attitude towards COVID-19 infection, and practice towards infection control were explored. Despite good knowledge levels on COVID-19 related infection and symptoms, around 40%-60% of the professionals were reluctant in providing audiological services to individuals who were asymptomatic. This study focused specifically on how COVID-19 had an effect on service delivery among audiologists and speech language pathologists. The tele-audiological practice/ perception among audiologists were not the purview of this study.
Indian Speech and Hearing Association (ISHA) is the professional and scientific association of speech language pathologists and audiologists in India [11]. It’s the national regulatory body that promotes and governs excellence in speech language and hearing profession. ISHA had mentioned that tele-practice could be a feasible option during the pandemic of COVID-19 and has formulated guidelines for tele-audiology practice in India. The specific difference and outstanding remark of the current study from the existing literature is that the KAP survey questionnaire was developed based on the teleaudiology guidelines provided by ISHA. Thus, the aim of the current study is to determine KAP regarding tele-audiology among audiologists in India.
This is a cross-sectional survey design conducted from 31st March to 17th May 2021. The study was approved by the Institutional Ethics Committee (REF: CSP/20/DEC/88/24), Sri Ramachandra Institute of Higher Education and Research (deemed to be University).
A KAP survey questionnaire was developed in English based on the ISHA guidelines of tele-practice [11]. The questionnaire for the survey consists of four domains with a total of 33 questions Supplementary Material (in the online-only Data Supplement). The domains include: demographic information, KAP on tele-audiology. The questionnaire was validated (content & construct validity) by two experts in tele-audiology practice with a minimum experience of 10 years and one research expert in KAP surveys. Based on the recommendations and suggestions provided by the experts; the questions were rephrased and rearranged. The ‘demographic’ domain comprised of questions related to educational qualification, place of work, work setting, and work experience in the area of tele-audiology. The ‘knowledge’ domain consisted of questions that focus on audiologist’s knowledge towards tele-audiology. Participants had to choose one among the three options (Yes/No/Don’t know). The ‘attitude’ domain comprised of five questions exploring the perception and attitude of tele-audiology among audiologists. ‘Practice’ referred to the ways in which the respondents demonstrate their knowledge and attitude through their actions. This domain contained questions that aid in gaining the audiologists willingness to practice tele-audiology, the most frequently used modality in practicing tele-services (such as synchronous, asynchronous, hybrid), the advantages of tele-practice and the challenges faced while providing tele-audiology. In both attitude and practice domain, the participants had to choose one among four choices, such as Likert-type questions. Mainly, frequency (Always/Often/Sometimes/Never) and agreement (Strongly disagree/Disagree/Agree/Strongly Agree) scales were included. It has one open-ended question to profile the respondents’ thoughts on comparing service delivery through tele-mode and face to face services.
The questionnaire was converted to an e-survey and weblink was distributed through Sri Ramachandra Speech and Hearing Alumni Association and ISHA. One hundred eight filled questionnaires were obtained in the database from 31st March 2021 to 17th May 2021. Out of the 108 respondents, 70 responses were from non-telepractitioners, and the remaining 38 responses were from the tele-practitioners. All the domains were filled by tele-practitioners, whereas the non-telepractitioners filled all domains except the practice domain.
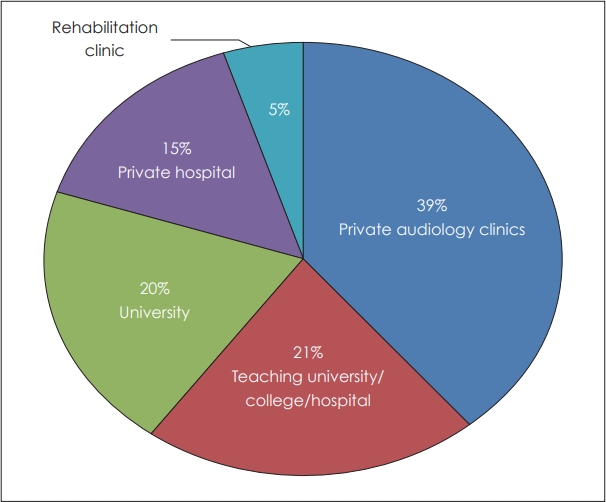
Of the 108 participants, 69.5% were females, and 30.6% were males. The mean age of the participants was 27 years (range: 22-52 years). Study partipants were from different states of India, and the responses were categorized based on zones. Maximum responses (80.4%) were from the southern zone of India. This was followed by responses from the central zone (14.0%) and northern zone (2.7%). The remaining responses were from the eastern zone (1.8%) and western zone (0.9%) of India. Study participants were from different employment types/work setting (Fig. 1).
Concerning the years of practicing tele-services, among the 38 participants, nearly half of the participants (44.7%) reported of tele-practice only during the pandemic of COVID-19; an additional one-quarter of participants (23.7%) reported that they provided tele-services for less than 10 years. The remaining participants reported less than 5 years (18.7%) and less than 2 years (13.2%) for practicing tele-audiology. Audiological services provided by tele-practitioners through tele-mode are represented below in Table 1.
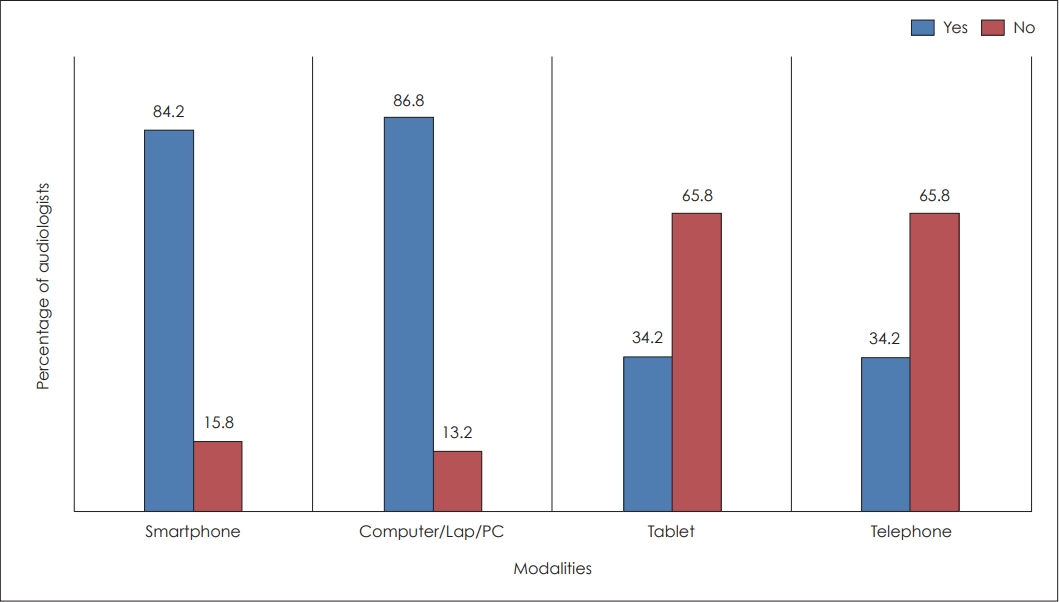
Most of the tele-practitioners reported using tele-health for counselling (27.5%) and therapeutical services (18.9%). In contrast, very few respondents indicated the usage of diagnostic testing such as distortion product otoacoustic emission testing (0.8%), auditory brainstem response testing (2.5%) and tinnitus evaluation (1.7%). The core diagnostic audiological tests were less conducted in tele-mode by many audiologists even during the pandemic. While analysing the responses on the modalities used in providing tele-services, the results demonstrated a clear preference for using smartphones and computers (Fig. 2). More than half of the audiologists preferred using fibre optic cables in providing tele-audiological services.
The knowledge section comprises of nine questions, and the results of each question are as follows.
Among the tele-practioners, 63.2% were aware of the tele-practice guidelines given by the ISHA. One-quarter of the participants (36.9%) were not aware or didn’t know about the tele-practice guidelines. Whereas among the non-telepractioners, 68.6% were aware of the tele-practice guidelines, and the remaining 31.5% of the participants either didn’t know or were not aware of the ISHA guidelines on tele-practice in India.
More than three-quarter (94.7%) of the tele-practioners stated that informed consent was mandatory before commencing tele-practice and the remaining (5.3%) of the participants stated that they didn’t know. Among the non-telepractitioners, 94.3% of them reported a strong need for informed consent before commencing tele-practice, and the remaining (7.5%) audiologists reported of either ‘No’ or ‘Don’t know’.
Selecting a videoconferencing platform based on the available bandwidth requirement at the audiologist end played a vital role in reducing the network challenges faced by the professionals. Around three-quarter of the tele-practioners (76.3%) reported ‘Yes’ to this statement, while (13.2%) of participants denied this statement, and the remaining (10.5%) were not sure about their answer. Of the 70 non-telepractitioners, 71.4% stated ‘Yes’ for this statement. The remaining (2.9%) reported ‘No’, and 25.7% were not sure about the answer.
ISHA guidelines to tele-practice [11] stated that a qualified ASLP should supervise tele-practice. All the tele-practitioners participated in the current study responded ‘Yes’ to this statement. Whereas among the non-telepractitioners, 91.4% reported ‘Yes’, and 8.6% responded as ‘No’ and ‘Don’t know’ to the statement.
The selection of remote computing software for providing tele-services is crucial. ISHA [11] recommends the use of software that explicitly provides details regarding data encryption, data protection and privacy. It was observed that almost 60.5% of tele-practitioners were aware of the usage of the remote computing software. The remaining one-quarter of the participants (23.7%) reported ‘Don’t know’, and 15.8% reported ‘No’ to this statement. Among the non-telepractitioners, more than three-quarter (75.7%) of the respondents reported ‘Yes’, following 20.0% who reported ‘Don’t know’, and 4.3% who reported ‘No’.
Among the tele-practitioners, 94.7% believed that an optimal environment at the patient end was a prerequisite for ideal tele-practice. While considering the non-telepractitioners, 88.6% agreed to the statement, and the remaining 11.0% either reported ‘No’ or ‘Don’t know’.
The ISHA guidelines on tele-practice [11] have stated that providing cross-border tele-practice without a license is beyond scope. Nearly 68.4% of the tele-practitioners reported ‘Yes’ to this statement; one-quarter of the participants (31.6%) reported either ‘Don’t know’ or ‘No’ to the statement. About 74.3% of the non-telepractitioners agreed to the statement related to cross-border tele-practice.
Sixty five percentage of tele-practioners reported that no specialized certification is required for providing tele-audiology in India, whereas the remaining 23.7% and 13.2% reported ‘Don’t know’ and ‘Yes’, respectively. Mixed responses were observed among the non-telepractitioners where 44.3% reported of no certification is required and the remaining reported of either ‘No’ or ‘Don’t know’.
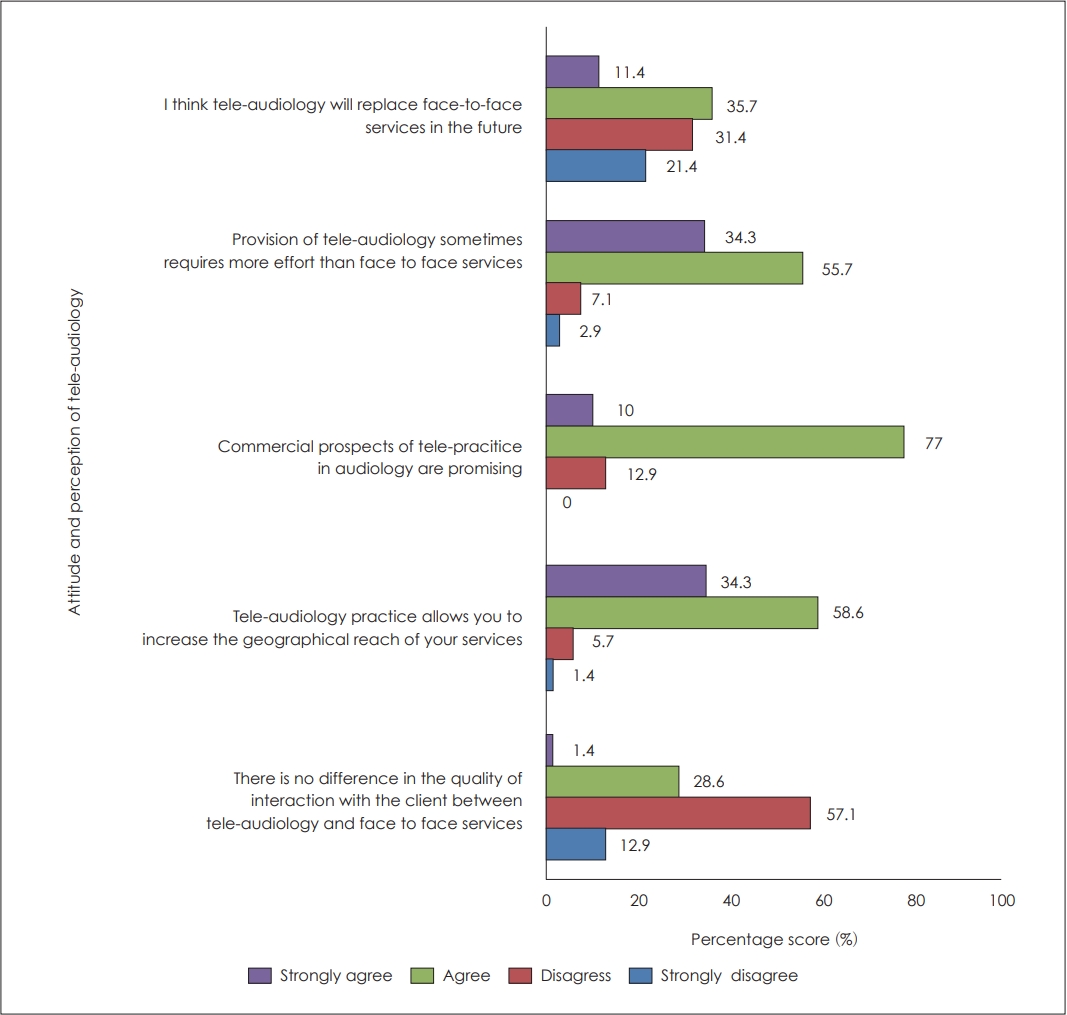
The responses obtained in this domain aids to measure the audiologists’ attitude and current perception towards tele-audiological services. Figs. 3 and 4 illustrates the summary of audiologist’s attitude towards tele-audiology among the tele-practitioners and non-telepractitioners.
Majority of the audiologists had a positive attitude that tele-practice increases the geographical reach of services. However, many participants didn’t show a positive attitude on the quality of interaction between the clinician and client in telemode. Half of the respondents disagreed with the statement that tele-practice would replace face to face service in future. Mixed opinion was observed regarding the future perspective of tele-audiology due to the opportunities and challenges faced by the providers. Reduced acceptance towards novel technologies, fear of handling patients via tele-practice, requirement of planning before commencing tele-sessions, high expectations on tele-practice and economic wellbeing of the audiologist are some of the reasons reported behind the negative perception of tele-audiology.
Questions concerned with the practice of tele-audiology were filled only by the telep-ractioners. More than half of the tele-practitioners (78.9%) reported that they practice tele-audiology ‘Sometimes’, followed by (15.8%) who reported of practicing ‘Often’ and (2.6%) reported of practicing ‘Always’. Tele-practitioners reported of serving a fairly balanced population of pediatric, adult, and geriatric patients. Fig. 5 illustrates the spread of the population served by the audiologist through tele-audiological services.
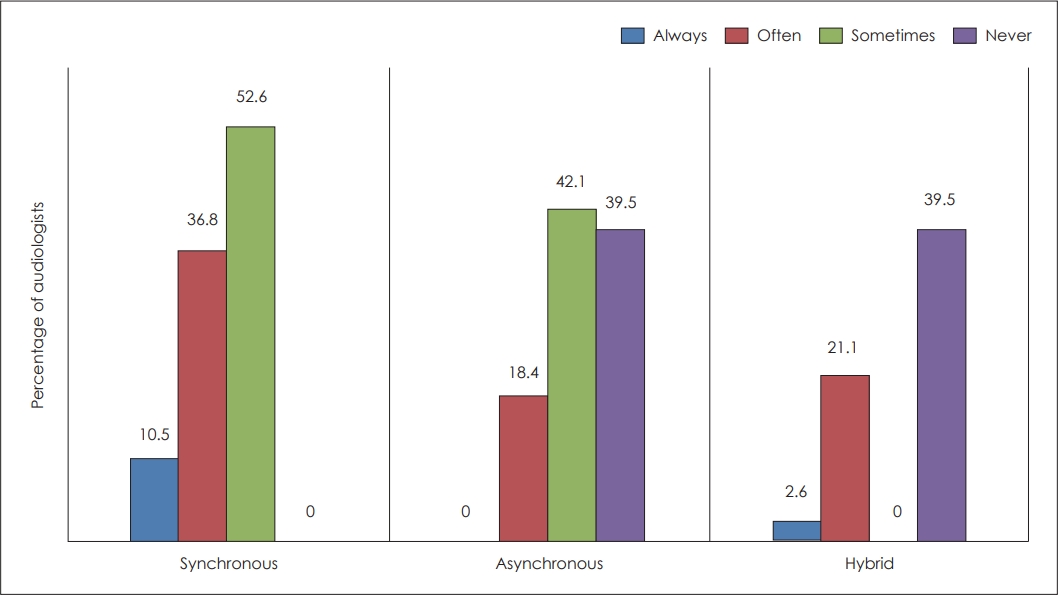
Majority of the tele-practitioners used synchronous (52.6%) and asynchronous (42.1%) models ‘Sometimes’ in providing tele-audiological services. 21.6% of tele-practitioners reported using the synchronous model ‘Often’ in their practice. Models used in the provision of tele-audiology are depicted in Fig. 6.
In tele-audiology, a facilitator is needed at the patient site to help with hands-on aspects of the tele-audiological procedures. From the current study results, it was identified that tele-practitioners ‘Sometimes’ used audiologists (28.9%), technicians (26.3%) and community health workers (23.7%) as patient site facilitators. More than half of the practitioners reported that they ‘Never’ use community health worker (65.8%) and community health nurse (76.3%) as facilitators in their practice.
Factors that tele-practitioners felt would the use of tele-audiology practice were explored (Table 2). Among the listed factors, equipment maintenance and loss of network were the ‘Often’ reported challenges by the tele-practioners. More than half of the tele-practitioners (60.5%) believed that tele-audiology reduces travel cost and reduced wait time (Table 3).
The study examined the KAP regarding tele-audiology among audiologists in India.
This domain elicited responses about the awareness of professional guidelines in providing tele-practice in India, awareness towards unethical practices and knowledge on the requirements needed in providing optimum service delivery. ISHA [11] has published guidelines of tele-practice for audiologists to consider during their service delivery. More than half of the tele-practioners and non-telepractioners reported of being aware of the tele-practice guidelines. This pandemic would have made many clinicians explore tele-practice and look into the guidelines to provide the best service. But more than one-third of the respondents were either not aware or didn’t know of such guidelines. Including the tele-practice guidelines in the curriculum may help many graduates to learn about the code of ethics and guidelines on tele-audiology.
Selecting a videoconferencing platform based on the available bandwidth requirement at the audiologist end plays a vital role in reducing the network challenges faced by the professionals [12]. Only around 70% of the respondents have agreed to this statement. Sufficient bandwidth is required for good quality videoconferencing. However, store- and forward-modes of tele-health require low bandwidth [13]. The audiologists should have sufficient knowledge in selecting the videoconferencing platform depending upon the available bandwidth in their environment.
It was interesting to know that all the tele-practitioners and 90% of non-telepractitioners were aware that a qualified ASLP should supervise tele-practice sessions. This is applicable especially when providing tele-services in remote areas where a local community health worker will be the test assistant. They are not qualified to make a diagnosis or interpretation; however, they are eligible to facilitate the information exchange between the patient and clinician with training. In this case, it is very important that an ASLP supervises and provides continued training and support to the local personnel [13].
Not majority of the tele-practioners were aware of the essentialness of the remote computing software during tele-testing. The tele-practitioners must be well aware of the software requirements used for patient testing/diagnosis. Videoconferencing software should be secure, and the software should access the remote computer and be compatible for audiological devices such as otoscope, audiometer, etc. [12]. As patient privacy and security are important aspects of health care delivery, care should be taken to comply with laws/acts regarding the same. Audiologists should be updated on the recent regulations to ensure patient privacy and security. The majority of the respondents were aware of the knowledge aspect related to malpractice and misconduct in tele-practice. These aspects are clearly discussed in the ISHA [11] code of ethics.
Most of the respondents believed that an optimal environment at the patient end is a prerequisite for ideal tele-practice. Environmental conditions on the patient end can affect the quality of tele-service. The patient environment should ensure privacy to avoid unauthorized access, and also the seating and lighting should be appropriate for both professional interaction and comfort. Very minimal background noise and lack of distraction at the patient end enhances the successful tele-practice. Not many of the respondents were aware of the international guidelines in providing tele-audiology. According to ISHA [11] , providing cross-border tele-practice without a license is beyond scope. Compliance with state licensure laws should be followed while providing tele-audiological services. As the regulations, laws, and policies for tele-health may vary across countries. Audiologists should be vigilant to stick to each country’s policies.
There was a mixed opinion on the knowledge question related to the requirement of specialized certification in providing tele-audiology in India. Around 40% of the respondents reported of don’t know, or no certification is required. Ravi, et al. [8] revealed that 90% of the tele-practitioners were interested in increasing their knowledge and wanting additional training and 75% of the non-telepractitioners were also interested in additional training to provide tele-audiology and to increase their knowledge. American Speech-Language-Hearing Association (ASHA) [5] conducted a survey on tele-practice among the practitioners and non-practitioners of tele-services. The survey results revealed that 43% of the non-telepractitioners expressed that they need more knowledge about tele-practice. The present study revealed that the respondents possess higher knowledge scores in majority of the knowledge questions. However, they lacked knowledge in few aspects, such as the essentialness of remote computing software, national and international guidelines on tele-services.
This section explored audiologists’ attitude towards the provision of tele-practice, quality of interaction in tele-practice, accessibility and future perspective of tele-audiology among the tele-practitioners and non tele-practitioners. More than three-quarters of the respondents exhibited a negative attitude towards the quality of interaction with the client within telepractice and face-to-face services. There are several reasons for this observed pattern of opposing attitude on the effect of tele-audiology on quality of interaction. Few of the reason could be due to technical issues such as internet breakdown, difficulties in communicating with hard of hearing patients, especially due to the lack of non-verbal cues, and in few instances due to the fear of technology. Practitioners experience in using information technology with the patients greatly influences the quality of interaction. Audiologists who have used informational technologies such as email/home-based software and apps are more likely to report a positive attitude towards the quality of interaction in tele-mode. A similar view has been reported by Hanson, et al. [14] who stated that first-time users of tele-technologies develop more positive attitudes with experience. Professionals who are not ready to explore/accept novel technologies and who fear of risks in applying newer technologies may not show a positive attitude towards quality of interaction in tele-mode. Singh [7] and Saunders [9] in their study, reported an adverse effect observed among the audiologists in quality of interaction in tele-audiology.
Majority of the audiologists indicated that tele-audiology would have a positive effect on the accessibility to services and increases the geographical reach of services. This is in line with previous literatures, which has stated that tele-audiology plays a vital role in improving the reach of audiological services to underserved communities [1,12,15-17]. More than three-quarter of the participants believed that commercial prospects of tele-audiology are promising. As audiological practice is highly reliant on computer-operated equipment and devices for screening, diagnosis and intervention, compatibility of these with the remote computing software has to be taken care of. Also, installing and maintaining the high-speed network lines such as LAN, ISDN, ADSL, satellite and method of managing the data/records involves high-cost factor. Our study finding is in line with the ASHA survey on the use of tele-practice, which states that 24% of the non-practitioners believed cost as a barrier in initiating tele-practice in their service delivery [5]. In contrast, Crowell, et al. [18] have stated that costs incurred with the remote hearing assessment are equal to those of a standard audiometric setup; these findings highlight that the economic consideration of tele-audiology tends to be unaffected while comparing with in-person testing. However, in the current study audiologists believed that the cost of delivering tele-audiology has adverse effects on their practice.
Nearly 90% of the tele-practitioners and non tele-practitioners agreed that tele-audiology sometimes required more effort than face-to-face service. The practitioners were asked to fill an open-ended question to profile their perception of teleaudiology comparing with face-to-face services. The respondents stated that a greater amount of planning was required before commencing tele-services, especially in the pediatric population. This notion is observed as they allocate more time in planning tele-sessions to gain better outcomes and to resolve technical problems caused by network issues during their practice [19] . More recently, in a study of Vrinda and Reni [20], practitioners believed difficulty in handling client through tele-practice is a common reason for preventing themselves from adopting tele-health.
Both the tele-practitioners and non tele-practitioners expressed mixed opinion towards the replacement of tele-audiology within face-to-face services. Half of the respondents believed tele-practice would replace face-to-face in the near future, and the other half denied the same. Many practitioners have stated that “tele-practice is a viable option not only during the COVID-19 and also beyond that”. Tele-audiology would enable the patients to be in more frequent contact with their audiologists or hearing health care providers. For instance, any issues or query related to the operation of a hearing aid/cochlear implant can be quickly solved in tele-mode rather than requiring to schedule face to face appointment. In recent years, many hearing-aid manufactures have incorporated tele-audiology features in their programming software so that adjustments can be carried out during remote tele-consultations. Though there are some disadvantages in carrying out few services such as ear mould modifications, tele-audiology provision should be considered on a case-to-case basis. Many authors have stated that tele-services are no different from in-person service delivery [17,18,21]. However, mixed results can also be due to the opportunities and challenges faced by the audiologist through tele-practice.
Despite the respondents being familiar with and willing to use tele-technologies, very few have adopted it for consultation/practice. The majority of the tele-practioners reported that they sometimes practice tele-audiology, and less than one-third of the tele-practitioners reported practicing often/always. For the consistent use of tele-audiology, infrastructure and systems need to be in place. Sometimes due to the high caseload and shortage of audiologists in audiology clinics, including tele-health services are considered as an added workload. Due to the barriers and challenges faced by the tele-practitioners, providing tele-audiology as a service delivery in their practice occurs at a lesser extent.
Nearly half of the respondents included synchronous mode in their practice, whereas asynchronous and hybrid models are quite less. This could be because many audiologists restrict tele-practice to counselling, or providing aural rehabilitation/therapy. As synchronous tele-health provides a direct and live connection between the patient and clinical site and often doesn’t require any additional infrastructure or additional training, this mode may be preferred among the tele-practioners in the current study. Counselling, hearing aid fitting, and programming, aural rehabilitation therapy were some of the services provided by the tele-practitioners of the current study using synchronous mode. This is in line with few other literatures [6,22]. Asynchronous tele-health requires health care workers/facilitators’ assistance at the remote location in facilitating clinical data transfer and addressing the challenges faced when conducting audiological testing. Owing to the difficulties in the availability of remote staff in the specific geographical area and lack of training sometimes may make it difficult to use asynchronous mode of service delivery.
Regarding the population served using tele-audiology, a fairly balanced population of pediatric, adult and geriatric patients were served via tele-audiology. But 30% of practitioners reported of ‘never’ provided tele-practice for the pediatric population. Some of the possible reasons for this negation could be due to the requirement of comprehensive audiological services, which may be lacking in many of the centres, difficulty in carrying out the testing due to poor rapport building or sometimes the parent’s unwillingness towards their child being tested in tele-mode [9,19]. Studies on the efficacy and feasibility of audiological services through tele-mode on various populations are required for the successful implementation of tele-program in comprehensive audiological care. Few of the Western literature had reported of positive attitude towards tele-rehabilitation. Brännström, et al. [23] evaluated audiologists and patient’s perception towards tele-audiology internet support for first time hearing aid users to understand the quality of content, ease of navigation and benefit from the program. Patients had expressed satisfaction and positive view towards the same. Beukes, et al. [24] explored patient satisfaction following tinnitus intervention and reported that both patients and audiologists reported higher satisfaction levels with the remote rehabilitation.
A facilitator at the patient end is needed to help with hands-on aspects of procedures. One-third of respondents reported choosing an audiologist followed by technicians. Majority of the respondents reported of not utilizing the community health nurse and community health worker as the facilitators. In many instances, an audiologist would not have required the assistance of a patient-site facilitator as the tele-audiological services were very much limited to counselling and aural rehabilitation. Similar reasons were also reported by Coco, et al. [25].
There are various factors that are reported by the audiologists that are likely to influence the tele-practice. Equipment maintenance and loss of network were the often reported challenges faced by the tele-practitioners. Tele-practice requires the use of equipment and software that is not ordinarily used for face to face testing. Additional training is required to use and troubleshoot the equipment. Adequate network support is required both at the patient and clinician site as higher speed and good bandwidth support are needed for diagnostic testing and videoconferencing. Several literatures have revealed that network crisis at the patient-end/providers end may cause the unsuccessful implementation of tele-practice [12,26]. Vrinda, et al. [20] stated that 94% of the tele-practitioners report internet connectivity issues as a major technical challenge during their practice; these findings comply with the present study results. These issues can be addressed by selecting the optimal source (network lines) and sticking to the videoconferencing software applications listed by ISHA [11]. Patient confidentiality in tele-health is reported to be the least affected factor in providing tele-health among the practitioners. The current study findings are in coherence with the ASHA survey on tele-practice [5]. It is important that tele-practitioners should be familiar with the legal frameworks on data privacy and protection, standard of care, consent, misconduct, malpractice and cross-border tele-practice guidelines outlined by ISHA [11].
Unsurprisingly, very few respondents reported that patient refused tele-service because of cost. This can be due to the lack of funding availabilities in procuring tele-health consultations by the government and are also due to the perceptions of people regarding online testing. More than 70% of the practitioners stated that tele-audiology reduces travel cost and time, reduces loss to follow up among the clients, reduces wait time and aids in serving patients at a larger distance. Due to COVID-19, several national restrictions and self-quarantine policies and protocols are in place. These seriously restrict the movement of the patient as well as follow-up visits are impossible. Tele-audiology has become a very good substitute enabling online consultations and follow-up evaluations. Favourable results concerning the loss of follow up with the client in face-to-face testing were reported to be overcome via tele-practice. Previous researchers have also stated the same [1,2]. However, regarding the cost of delivering tele-audiology, many respondents expressed a neutral belief which could be due to a lack of knowledge about the infrastructure requirements in constructing and conducting tele-practice.
Inspite of good knowledge skills and attitude on tele-audiology, the application/practice of tele-audiological services is very much limited. Changes in health care model are essential during this pandemic. In a recent systematic review of contemporary tele-audiology, 10 checklists were suggested for planning/implementing tele-audiology practice [27]. Further, evidence based practices on comprehensive pediatric testing and other diagnostic test battery using tele-mode is warranted.
From the current study, it is clear that the acceptance of tele-practice in India among audiologists has improved post COVID pandemic. Though majority of the audiologists possess good knowledge and positive attitude towards tele-audiology, there still exists a gap in the actual use/practice of tele-audiology. The application/practice of tele-audiology were very much limited to counselling, therapy for hearing impairment and troubleshooting of hearing aid devices. Use of diagnostic audiological testing in tele-mode is limited even during this pandemic. Evidence based practices on conducting diagnostic test battery in tele-mode, hands-on training on running diagnostic tests battery/rehabilitation using tele-mode, improving knowledge on technical requirements for tele-practice may yield a greater positive perception and practice of tele-audiology among the audiologists. Specialised training and continuing education programmes on tele-practice should be regularly conducted to facilitate the use of tele-mode in service delivery. Audiologists should consider using tele-audiology to ensure continuous and uninterrupted access to audiological services. This provision should be made available in a variety of clinical settings.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.7874/jao.2021.00584.
Supplementary Material
Knowledge, Attitude and Practice of tele-audiology – Audiologist
Acknowledgments
The authors acknowledge the audiologists who had participated in the study and also the professional bodies in facilitating invitations to their members and the respondents to the survey.
Notes
Author Contributions
Conceptualization: Jayashree Seethapathy. Data curation: Nazreen Nihara M R. Formal analysis: Nazreen Nihara M R, Jayashree Seethapathy. Investigation: Nazreen Nihara M R. Methodology: Jayashree Seethapathy, Nazreen Nihara M R. Project administration: Nazreen Nihara M R. Resources: Jayashree Seethapathy, Nazreen Nihara M R. Software: Nazreen Nihara M R, Jayashree Seethapathy. Supervision: Jayashree Seethapathy. Validation: Jayashree Seethapathy. Visualization: Nazreen Nihara M R. Writing—original draft: Nazreen Nihara M R. Writing—review & editing: Jayashree Seethapathy. Approval of final manuscript: Jayashree Seethapathy.
Table 1.
Audiological services provided in tele-mode
Table 2.
Factors affecting tele-practice in providing audiological services
Table 3.
Advantages of providing tele-audiology
REFERENCES
2. Dharmar M, Simon A, Sadorra C, Friedland G, Sherwood J, Morrow H, et al. Reducing loss to follow-up with tele-audiology diagnostic evaluations. Telemed J E Health 2016;22:159–64.


3. Eikelboom RH, Swanepoel W. International survey of audiologists’ attitudes toward telehealth. Am J Audiol 2016;25(3S):295–98.


4. Ramkumar V, Selvakumar K, Vanaja CS, Hall JW, Nagarajan R, Neethi J. Parents’ perceptions of tele-audiological testing in a rural hearing screening program in South India. Int J Pediatr Otorhinolaryngol 2016;89:60–6.


5. American Speech-Language-Hearing Association. Survey report on telepractice use among audiologists and speech-language pathologists. Rockville: American Speech-Language-Hearing Association;2002.
6. Mohan HS, Anjum A, Rao PKS. A survey of telepractice in speech-language pathology and audiology in India. Int J Telerehabil 2017;9:69–80.




7. Singh G, Pichora-Fuller MK, Malkowski M, Boretzki M, Launer S. A survey of the attitudes of practitioners toward teleaudiology. Int J Audiol 2014;53:850–60.


8. Ravi R, Gunjawate DR, Yerraguntla K, Driscoll C. Knowledge and perceptions of teleaudiology among audiologists: a systematic review. J Audiol Otol 2018;22:120–7.



9. Saunders GH, Roughley A. Audiology in the time of COVID-19: practices and opinions of audiologists in the UK. Int J Audiol 2021;60:255–62.


10. Gunjawate DR, Ravi R, Yerraguntla K, Rajashekhar B, Verma A. Impact of coronavirus disease 2019 on professional practices of audiologists and speech-language pathologists in India: a knowledge, attitude and practices survey. Clin Epidemiol Glob Health 2021;9:110–5.



11. Indian Speech and Hearing Association. Telepractice guidelines for audiology and speech language pathology services in India [Internet]. [cited 2021 September 10]. Available from: https://www.ishaindia.org.in/downloads/Tele-PRACTICE-GUIDELINES.pdf.
12. Ballachanda B. Critical steps in establishing a teleaudiology practice. Hearing Review 2017;24:14–7.
13. Eikelboom RH, Swanepoel DW. Tele-audiology. editors. The E-Medicine, E-Health, M-Health, Tele-medicine, and Tele-health Handbook. Tele-medicineand Electronic Medicine. In: Eren G, Webster JG. Boca Raton: CRC Press;2016. p.539–60.
14. Hanson D, Calhoun J, Smith D. Changes in provider attitudes toward telemedicine. Telemed J E Health 2009;15:39–43.


15. World Health Organization. Coronavirus disease (COVID-19 pandemic) [Internet]. [cited 2021 September 10]. Available from: URL: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
16. Thrum M, Driscoll C, Keogh T. Investigating the satisfaction of clinicians and clients in a teleaudiology trial. J Hear Sci 2018;8:34–47.

17. Swanepoel de W, Hall JW 3rd. A systematic review of telehealth applications in audiology. Telemed J E Health 2010;16:181–200.


18. Crowell ES, Givens GD, Jones GL, Brechtelsbauer PB, Yao J. Audiology telepractice in a clinical environment: a communication perspective. Ann Otol Rhinol Laryngol 2011;120:441–7.



19. Akamoglu Y, Meadan H, Pearson JN, Cummings K. Getting connected: speech and language pathologists’ perceptions of building rapport via telepractice. J Dev Phys Disabil 2018;30:569–85.


20. Vrinda R, Reni PS. Telerehabilitation in the field of speech language pathology during pandemic Covid19 outbreak-an analysis in Kerala. Biosci Biotechnol Res Commun 2020;13:2281–8.

21. Ramkumar V, Hall JW, Nagarajan R, Shankarnarayan VC, Kumaravelu S. Tele-ABR using a satellite connection in a mobile van for newborn hearing testing. J Telemed Telecare 2013;19:233–7.



22. Yashaswini R, Rao PKS. Tele speech-language pathology and audiology in India-A short report. JISfTeH 2018;6:e19.
23. Brännström KJ, Öberg M, Ingo E, Månsson KNT, Andersson G, Lunner T, et al. The initial evaluation of an internet-based support system for audiologists and first-time hearing aid clients. Internet Interv 2016;4:82–91.



24. Beukes EW, Allen PM, Manchaiah V, Baguley DM, Andersson G. Internet-based intervention for tinnitus: outcome of a single-group open trial. J Am Acad Audiol 2017;28:340–51.


25. Coco L, Davidson A, Marrone N. The role of patient-site facilitators in teleaudiology: a scoping review. Am J Audiol 2020;29(3S):661–75.



- TOOLS