Recurrent Benign Myoepithelioma of the Auricle
Article information
Abstract
Myoepithelioma, a generally benign tumor comprised of myoepithlial cells, is an uncommon salivary gland tumor. Myoepithelioma originates primarily in the parotid gland, but several isolated cases have been described. Although myoepithelioma has a benign nature, but there is a potential risk of malignant change and recurrence in case of incomplete resection. We acknowledge that benign myoepithelioma originating from the auricle has not been reported in the English literature. We present a rare case of 27-year-old female who had recurrent benign myoepithelioma originating from the auricle and already had been given twice operations at the other clinic.
Introduction
Myoepithelioma is a benign neoplasm of salivary glands derived from myoepithelial cells. Myoepithelioma was initially considered to be a type of pleomorhpic adenoma,1) however today it is considered to be a relatively more aggressive tumor because it has higher recurrence or undergoing malignant transformation. Therefore, it is now regarded to be an independent entity according to the latest World Health Organization histologic classification of tumors of 2005. Four distinct cellular components have been described based on morphology: spindle, plasmacytoid, epithelioid, and clear cells; a wide variety of combined or intermediate forms are also seen.2) It is not easy to diagnose myoepithelioma with only using light microscopic examination, therefore immunohistochemical staining is useful for diagnosis. Myoepithelioma originates primarily in the parotid gland, but extra-parotid myoepithelioma has occurred in the breast, nasal cavity, nasopharynx, middle ear, and hard palate.3,4,5,6,7) We report a case of a 27-year-old female patient with benign myoepithelioma located in the auricular scaphoid fossa.
Case Report
A 27-year-old woman who had complained of slow growing painless nodular mass presenting in left auricle for 8 years was referred to our clinic. The mass had gradually grown and been accompanied by hardness. She had already twice operations at the other clinics, but soon recurred at that time. The mass was localized to upper scaphoid fossa of auricle (Fig. 1A). But the skin over the mass in the auricle was intact. Computed tomography and magnetic resonance imaging were not performed because we thought it as a simple tumor such as epidermoid cyst which is mainly occurred in the auricle.8) The tumor was removed en bloc uneventfully by surgical excision and thereafter, full-thickness skin graft which was har-vested at the ipsilateral retroauricular area was included to surgery (Fig. 1B). At surgery, the tumor was soft, well-encapsulated, and was easily separated from adjacent structures, such as conchal cartilage. After excision, the mass was measured 10×10×6 mm in dimensions (Fig. 2).
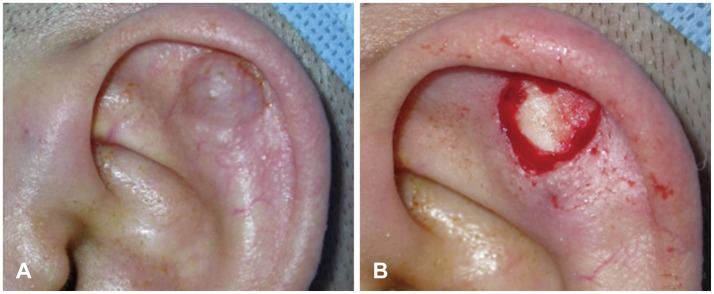
Operative findings. A: The mass was localized to scaphoid fossa of auricle. B: Surgical field following the removal of the specimen.

Gross specimen shows well-encapsulated pink-white soft tissue, measuring 0.2 g in weight and 10×10×6 mm in dimensions.
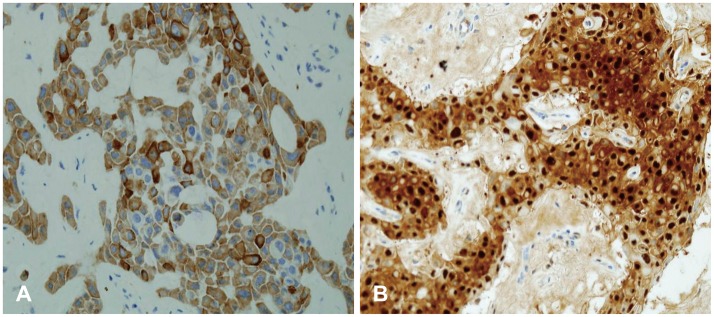
Histologically, the mass showed well-defined margins and was separated from overlying epidermis (Fig. 3). Epithelioid cells were arranged in nests and lobular pattern and embeded in hyalinization to chondromyxoid stroma. Myoid stroma was noticeable and it was considered to be close to the plasmacytoid cell type. The α-smooth muscle actin (SMA), epithelial membrane antigen (EMA), PanCK, S-100 protein and Ki-67 proliferation index in the tumor cells was demonstrated with immunohistochemical examination (Fig. 4). The PanCK, S-100 protein was diffusely positive, whereas SMA and EMA were negatively stained. Ki-67 proliferation index was stained less than 1%. The microscopic examination and immunohistochemical profiles were consistent with benign myoepithelioma. No complications were observed during the postoperative course, and the patient was discharged 7 days after surgery. The patient is clinically free of disease 18 months after surgery. The institutional review board of Pusan National University has approved this study.
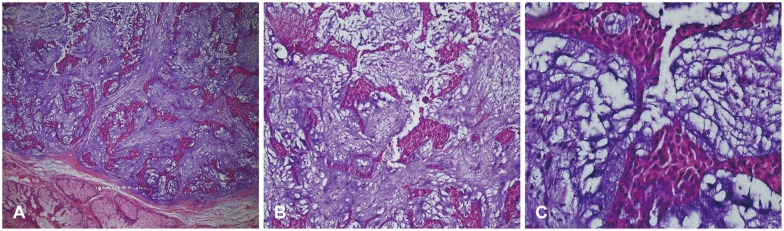
Histologic findings. A: The myoepithelioma is separated from overlying epidermis. B: Epithelioid cells are arranged in nests and lobular pattern and embeded in hyalinized to chondromyxoid stroma. C: There are few mitotic figure <2/10 HPF (original magnifications: A, ×40; B, ×100; C, ×400).
Discussion
Among the pathology of auricular mass, the most common type is epidermal cyst (25.3%), followed by hypertrophic scar (12.6%), fibrous tissue-accessory ear (9.5%), chronic inflammation-nevus (7.9%), keloid (6.3%), hemangioma (4.7%).9) Initially, this lesion was considered to be a benign tumor that was same type of pathology described above because the tumor appeared well demarcated on morphology. After excision of entire mass, the result of biopsy confirmed the myoepithelioma.
More than 200 cases of benign myoepitheliomas have been reported to date. To the best of our knowledge, benign myoepithelioma originating from the auricle has not been described in the literature to date. The cases of myoepithelioma present as painless, slowly growing, firm masses, usually of small size. This tumor can be occurred at any age, however it is most commonly occurred to young adults between the ages of 30 and 50, with average of age in 36.3 years.9) Within the benign myoepithelioma catergory, morphologically, 4 histopathologic subtypes have been well recognized. These include plasmacytoid, epithelioid, spindle, and clear cells, which can be associated with mucoid or hyalinized stroma. Less common cellular patterns, including basaliod and oncocytic, have also been reported.7) However, the histologic subtype has not seemed to influence the clinical and/or biologic behavior of these tumors. The most common subtype has been the spindle cell variant, usually seen in the parotid gland, with the plasmacytoid type predominantly seen in the hard palate. Each individual tumor includes areas with more than one growth pattern or cell subtype.10)
Myoepithelioma has clinical or biologic behavior similar to that of other benign salivary gland tumors. These are slow-growing, well-encapsulated or circumscribed, asymptomatic tumors that usually range from 1 to 5 cm in diameter. The tumor cut surface is usually uniform white, tan, or gray.
Immunoreactivity for S-100 protein is currently considered an important characteristric of this morphologic variant of myoepithelioma.1) Malignant transformation to myoepithelial carcinoma has been reported. A diagnosis of myoepithelical carcinoma should be considered if the tumor cells exhibit atypical or increased mitotic activity, necrosis, or cellular pleomorphism, with evidence of invasion into the adjacent anatomic tissue.11) Immunohistochemical staining also can help to differentiate between benign and malignancy. The cell proliferative activity estimated using Ki-67 labeling index is higher in malignant myoepithelioma of salivary glands than in benign myoepithelioma.12) In this case, Ki-67 proliferation index was stained less than 1%. Therefore, Ki-67 would be a useful prognosis marker for myoepithelioma.
There is no consensus regarding the optimal treatment for benign myoepithelioma because of its rarity, however as performed in the current case, surgery with a margin of normal uninvolved tissue being included within the surgical excision is the first choice of treatment for benign myoepitheliomas, and the recurrence rates are similar to those of the pleomorphic adenomas.13) The prognosis for benign myoepitheliomas is quite favorable with complete excision, but patients should undergo regular long-term following-up examinations to rule out local recurrence such as this case.14)