|
 |
- Search
| J Audiol Otol > Volume 23(3); 2019 > Article |
|
Abstract
Differentiating central vestibulopathy from more common vestibular disorders is crucial because it often necessitates different treatment strategies, and early detection can help to minimize potential complications. Isolated nodular infarct is one of the central brain lesions that can mimic peripheral vertigo. We present a case of isolated nodular infarct that had been misdiagnosed as vestibular neuritis on the contralateral side at the initial evaluation. The patient was successfully treated with anticoagulants and antihyperlipidemic agents. Clinicians should keep in mind that some causes of central vertigo mimic peripheral vestibulopathy at the early stage.
Vestibular neuritis (VN) is one of the most common causes of peripheral vertigo. Although there is no gold standard for the diagnosis of VN, the following conditions are regarded as essential: 1) the sudden-onset severe of vertigo lasting for at least 24 hours, 2) the absence of auditory symptoms or signs, 3) a direction-fixed horizontal-torsional unidirectional spontaneous nystagmus (SN) as observed with a Frenzel glass or infrared goggles, 4) a positive horizontal head impulse test (HIT), 5) the absence of positional nystagmus, 6) unilateral caloric hypo-excitability, and 7) negative neurologic examinations [1-4].
Patients with cerebellar infarction may have postural imbalance, disequilibrium, vertigo, and headache. Thus, they could be misdiagnosed with VN [5]. Therefore, detailed history taking, and precise vestibular function tests are essential for differential diagnosis, and further radiologic examination such as magnetic resonance imaging (MRI) or computed tomography (CT) scan may be necessary. However, a high rate of false negative radiologic exams in the early stage has been reported [6]. The false negative rate was reported to be up to 21% if the radiologic examination was performed within 24 hours.
We report a case of isolated nodular infarction that was previously misdiagnosed as VN on the contralateral side.
A 57-year-old male patient visited the emergency room complaining of acute vertigo that had started suddenly on the day of the visit. He had had hypertension and non-insulin-dependent diabetes for three years. In addition to vertigo, he had severe nausea, vomiting, and headache around the occipital area that couldn’t be controlled with acetaminophen. He told that he had experienced severe dizziness that was recovered spontaneously within a few days in the past.
The Frenzel glass test showed left beating SN and positive HIT on the right side. The Romberg test was not possible because of severe vertigo. However, there was no dysmetria in the finger-to-nose test. Brain CT angiography (CTA) and diffusion weighted brain MRI were performed to discriminate central origin vertigo. Neither acute brain hemorrhage nor recent infarction were observed.
The patient was diagnosed as having VN on the right side and admitted to the hospital. For treatment, dimenhydrinate 100 mg/day, diazepam 4 mg/day orally, intravenous metoclopramide 25 mg, and ginkgo biloba extract 17.5 mg were administered.
The left beating SN and the positive HIT on the right side were observed continuously until day 2. At day 3, gait disturbance became milder and both SN and the lateralizing sign of HIT disappeared. Therefore, the patient was instructed to do additional vestibular rehabilitation exercises.
On day 5, laboratory testing was performed. Sixty-two percent of caloric weakness on the left side was observed (Fig. 1). The fixation index, using the arithmetic means of warm stimulation, were 105% on the right, and 58% on the left, suggesting failure of fixation suppression on the right side. Both the subjective visual vertical and horizontal angles were rotated to 12° in a clockwise direction. In the rotatory chair test (RCT), mild asymmetry in sinusoidal harmonic acceleration (SHA) test was observed (Fig. 2); however, the step velocity test result was within the normal range. Similarly, the video head impulse test (vHIT) and vestibular evoked myogenic potential test were also normal (Fig. 3).
On the other hand, the patient complained of persistent subjective vertigo and occipital area headache. The severity of these symptoms became milder but then stayed the same after the small improvement. Thus, additional radiologic evaluation consisting of diffusion weighted MRI and magnetic resonance angiography was conducted. Subacute, isolated nodular infarction on the left side and a 3.2×2.7 mm dissecting aneurysm in the proximal part of the left posterior inferior cerebellar artery (PICA) were found (Fig. 4). Medications including anticoagulants and antihyperlipidemic agents were additionally prescribed, and the patient was discharged after 4 days of additional observation because vertigo and the occipital area headache had completely resolved.
This patient was misdiagnosed as having acute VN on the right side, because of observations of SN toward the left side, positive HIT on the right side, negative findings on diffusion weighted MRI and CTA, no audiologic symptoms, and negative neurologic results.
Among patients who visit emergency rooms complaining of acute vertigo, 0.7-3.2% have central origin vertigo [7]. In this case, the first diffusion weighted brain MRI showed a negative result, but the follow-up brain MRI obtained 5 days after onset of initial symptoms finally showed a left isolated nodular infarction.
This patient complained of a sustained occipital headache that did not respond to medical treatment. It has been noted that severe occipital headaches, dysarthria or dysmetria, are common symptoms of a PICA infarct [5]. Even in patients with benign paroxysmal positional vertigo, a severe headache can justify radiological imaging, in the same way that abnormal cranial nerve findings and visual disturbances can also justify an MRI [8]. In addition, the failure of fixation suppression on a caloric test was also later observed. Thus, in the emergency room, brain CT imaging and a diffusion weighted brain MRI were obtained in order to rule out the possibility of central vestibulopathy. However, all of the initial radiologic findings were normal.
A cerebellar nodulus is supplied in a multiple fashion by the medial side of the PICA and anterior inferior cerebellar artery and superior cerebellar artery [9]. Thus, isolated nodular infarction is very rare because of the abundant blood supply to the cerebellar nodulus. Through a literature review, the authors found that twelve cases of isolated nodular infarction had been reported during 2004-2018 (Table 1). In addition, a dissecting aneurysm of the PICA was reported to be associated with cerebellar infarction [10]. Considering these findings together, our patient’s nodular infarct might have been caused by the dissecting aneurysm at the proximal branch of the PICA.
Functionally, a cerebellar nodulus connects the peripheral vestibular system and central vestibular system. Thus, various symptoms ranging from ipsilateral SN, postural vertigo, and apogeotropic postural nystagmus to central signs such as ataxia can occur in cases of cerebellar infarction [9]. The cerebellar nucleus receives afferent fibers mostly from the vestibular nuclei, nucleus prepositus hypoglossi, inferior olivary nucleus, and vestibular nerve, whereas the main efferents project to the vestibular nucleus. In particular, Purkinje fibers, which connect the cerebellar nodulus and vestibular nuclei, deliver an ipsilateral inhibitory component [9].
This patient had a left beating SN and positive HIT on the right side at the initial visit. As the cerebellar nodulus delivers efferent inhibitory signals to ipsilateral vestibular nuclei via Purkinje fibers, loss of inhibition by cerebellar nodular infarction leads to hyperexcitability of the ipsilateral, left vestibular nuclei [9]. The static and dynamic imbalance between the bilateral vestibular nuclei might have resulted in this patient’s initial left beating SN and the positive HIT finding on the right side.
Considering the pathophysiology of the isolated nodular infarct, it would be more natural if this patient had had a right sided caloric weakness resulting from the disinhibition of the left vestibular nuclei. However, a previous review study also reported normal caloric test results, in similar circumstances, contrary to our assumptions [9]. Despite these previous findings, in this case study the patient exhibited a left sided caloric weakness. Because this patient had experienced severe dizziness in the past, we assumed that this finding might be explained by his previous peripheral vestibulopathy, but not by the present isolated nodular infarct.
On the other hand, this patient showed a mild asymmetry on the SHA test (Fig. 2). This differed from previous studies in that all reported normal findings in RCT [5,9]. It may well be that the findings indicated in this study are more persuasive than those of previous studies as the SHA test result correlates with SN.
Moreover, discrepancies between the results of the vHIT and bedside HIT was also observed. We assumed that this might have been caused by the passing of time. However, a bedside HIT was performed every day from the time of the patient's admittance to the emergency room, and the vHIT was performed on day 5. By day 5, both the SN, and the positive HIT on the frenzel glass test, had already disappeared following recovery. If vHIT had been performed earlier, we could have found similar pathological findings as with HIT. Consistent with our findings, others have observed that bedside HIT seems to be more meaningful in an emergency setting, and the clinical significance of gain-based vHIT may be limited [11-14].
Taken together, it has become apparent as to why the vestibular function test (VFT) findings, including the bed side examination at the emergency room, were different from that of a typical peripheral vestibulopathy. First, this patient had central vestibulopathy, thus the VFT results couldn’t help but be different from those of a peripheral vestibulopathy. Second, he had had a past medical history of severe vertigo that had resolved spontaneously, and this might have complicated the interpretation of the VFT findings. In short, this patient had central vestibulopathy combined with a previous history of peripheral vestibulopathy on the contralateral side.
In conclusion, clinicians may consider radiologic re-evaluation for a proper diagnosis if a dizzy patient has 1) discordance between the physical examination and symptoms, 2) a past medical history that includes hypertension and diabetes, and 3) persistent vertigo and headache that cannot be explained. For this, continued attention is also required after initial assessment.
Acknowledgments
This research was funded by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2017R1C1B5017839).
Notes
Authors’ contribution
Conceptualization: Ho Yun Lee. Data curation: Jun Lee and Kudamo Song. Formal analysis: Jun Lee and Kudamo Song. Funding acquisition: Ho Yun Lee. Investment: Ho Yun Lee. Methodology: Ho Yun Lee and In Kyu Yu. Project administration: Ho Yun Lee. Resources: Ho Yun Lee. Software: Ho Yun Lee. Supervision: Ho Yun Lee. Validation: Kudamo Song and Ho Yun Lee. Visualization: In Kyu Yu and Kudamo Song. Writing—original drift: Jun Lee. Writing— review & editing: Ho Yun Lee.
Fig. 1.
Results of caloric test performed on day 5. Note that left-sided caloric paresis was prominent. SPV: slow phase velocity.
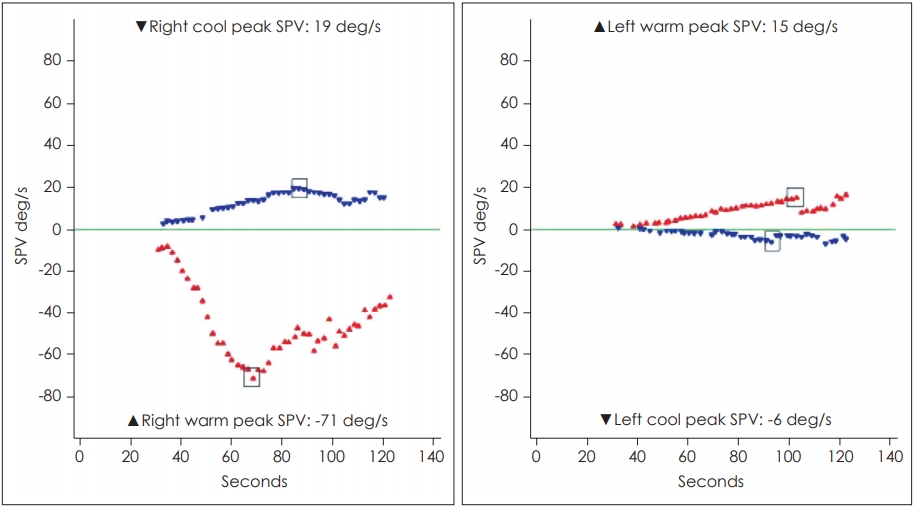
Fig. 2.
Results of the sinusoidal harmonic acceleration test performed on day 5. Mild asymmetry in sinusoidal harmonic noted whereas phase and gain were within normal limits.
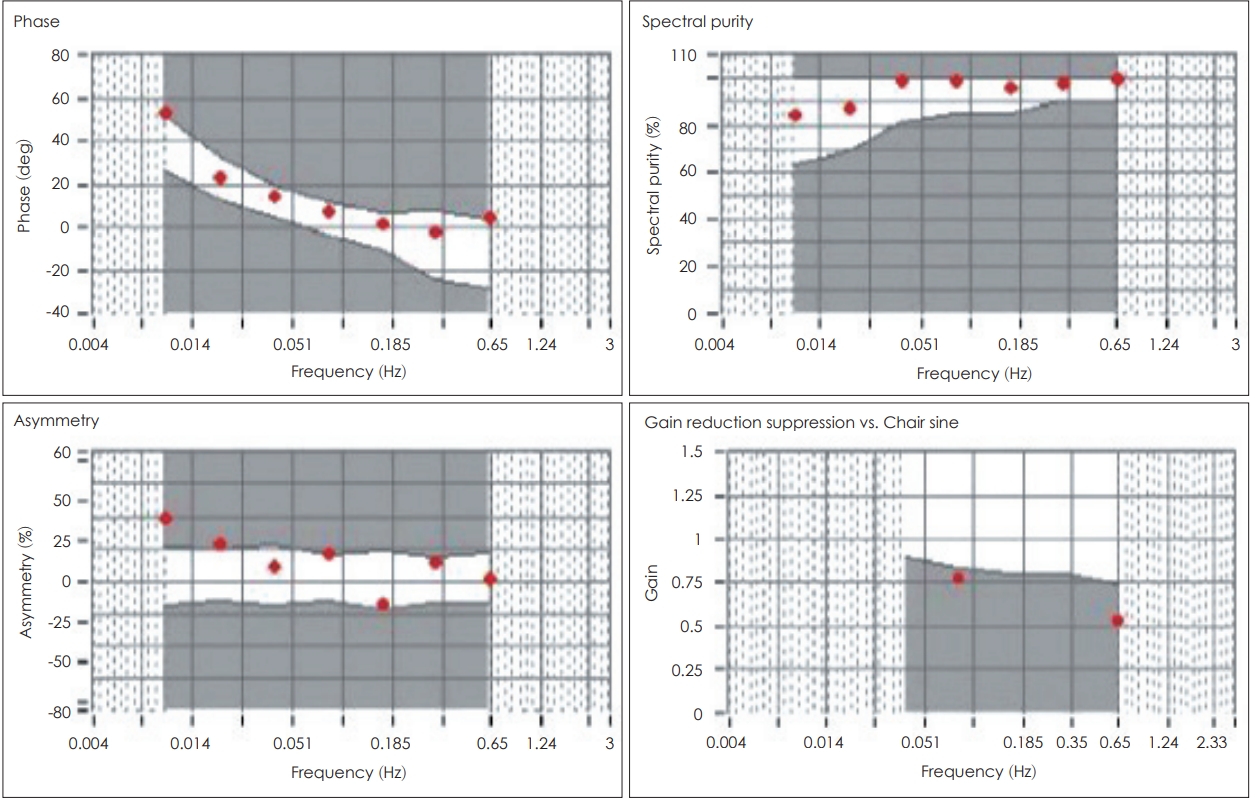
Fig. 3.
Results of the video head impulse test performed on day 5. Head impulse gain of all semicircular canals were within normal limits. LARP: left-anterior-right-posterior, RALP: right-anterior-left-posterior.

Fig. 4.
Radiologic findings of diffusion weighted magnetic resonance imaging and magnetic resonance angiography. (A) Cerebellar nodular infarct. White arrow indicates acute ischemic lesions of the cerebellar nodule. (B) Posterior inferior cerebellar artery (PICA) aneurysm. White arrow indicates 3.2×2.7 mm dissecting aneurysm in the proximal part of the left PICA.
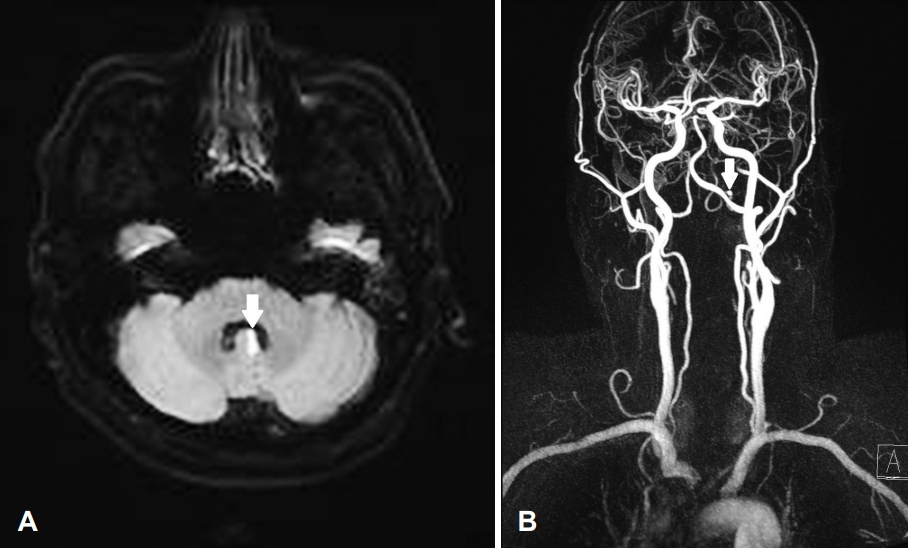
Table 1.
Systematic reviews of previous reports dealing with isolated nodular infarction
| No. | Reference | Age (years) | Sex | Lesion side | SN | Positional nystagmus | HIT | Associated symptom |
|---|---|---|---|---|---|---|---|---|
| 1 | Lee, et al. [5] | 37 | M | L | L | - | Normal | - |
| 2 | Moon, et al. [9] | 67 | M | Both | R/D | - | Normal | - |
| 3 | Moon, et al. [9] | 66 | F | R | R | - | Normal | - |
| 4 | Moon, et al. [9] | 51 | M | L | L | - | Normal | - |
| 5 | Moon, et al. [9] | 64 | F | L | - | DCPN (APO) | Normal | - |
| 6 | Moon, et al. [9] | 69 | M | Both | PAN | - | Normal | - |
| 7 | Moon, et al. [9] | 37 | M | L | L | - | Normal | - |
| 8 | Moon, et al. [9] | 75 | F | R | R | - | Normal | - |
| 9 | Moon, et al. [9] | 52 | M | R | R | - | Normal | - |
| 10 | Nam, et al. [12] | 36 | M | Both | - | DCPN (APO) | - | Ataxic gait |
| 11 | Kim, et al. [13] | 67 | F | Both | - | DCPN (APO) | - | - |
| 12 | Choi, et al. [14] | 58 | M | R | R | DCPN (APO) | - | Mild ataxic gait |
REFERENCES
2. Oron Y, Shemesh S, Shushan S, Cinamon U, Goldfarb A, Dabby R, et al. Cardiovascular risk factors among patients with vestibular neuritis. Ann Otol Rhinol Laryngol 2017;126:597–601.


4. Ahn SH, Shin JE, Kim CH. Final diagnosis of patients with clinically suspected vestibular neuritis showing normal caloric response. J Clin Neurosci 2017;41:107–10.


5. Lee H, Cho YW. A case of isolated nodulus infarction presenting as a vestibular neuritis. J Neurol Sci 2004;221:117–9.


6. Tong DC, Yenari MA, Albers GW, O'Brien M, Marks MP, Moseley ME. Correlation of perfusion- and diffusion-weighted MRI with NIHSS score in acute (<6.5 hour) ischemic stroke. Neurology 1998;50:864–70.


7. Nelson JA, Virre E. The clinical differentiation of cerebellar infarction from common vertigo syndromes. West J Emerg Med 2009;10:273–7.



8. Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, et al. Clinical practice guideline: benign paroxysmal positional vertigo (update). Otolaryngol Head Neck Surg 2017;156(3_ suppl):S1–47.

9. Moon IS, Kim JS, Choi KD, Kim MJ, Oh SY, Lee H, et al. Isolated nodular infarction. Stroke 2009;40:487–91.


10. Tawk RG, Bendok BR, Qureshi AI, Getch CC, Srinivasan J, Alberts M, et al. Isolated dissections and dissecting aneurysms of the posterior inferior cerebellar artery: topic and literature review. Neurosurg Rev 2003;26:180–7.



11. Guler A, Karbek Akarca F, Eraslan C, Tarhan C, Bilgen C, Kirazli T, et al. Clinical and video head impulse test in the diagnosis of posterior circulation stroke presenting as acute vestibular syndrome in the emergency department. J Vestib Res 2017;27:233–42.



12. Nam J, Kim S, Huh Y, Kim JS. Ageotropic central positional nystagmus in nodular infarction. Neurology 2009;73:1163