1. Saki N, Yadollahpour A, Moniri S, Karimi M, Bayat A, Abshirini H, et al. Investigating the impacts of cochlear implantation on the happiness and self-esteem of mothers of children with severe hearing loss. Int J Ment Health Addiction 2017;15:288–94.


2. Tomblin JB, Peng SC, Spencer LJ, Lu N. Long-term trajectories of the development of speech sound production in pediatric cochlear implant recipients. J Speech Lang Hear Res 2008;51:1353–68.


3. Ching TY, Dillon H, Day J, Crowe K, Close L, Chisholm K, et al. Early language outcomes of children with cochlear implants: interim findings of the NAL study on longitudinal outcomes of children with hearing impairment. Cochlear Implants Int 2009;10 Suppl 1:28–32.


4. Dowell RC, Dettman SJ, Blamey PJ, Barker EJ, Clark GM. Speech perception in children using cochlear implants: prediction of long-term outcomes. Cochlear Implants Int 2002;3:1–18.


5. Moog JS, Geers AE. Epilogue: major findings, conclusions and implications for deaf education. Ear Hear 2003;24(1 Suppl):121S–5S.


6. Sarant JZ, Blamey PJ, Dowell RC, Clark GM, Gibson WP. Variation in speech perception scores among children with cochlear implants. Ear Hear 2001;22:18–28.


7. Connor CM, Craig HK, Raudenbush SW, Heavner K, Zwolan TA. The age at which young deaf children receive cochlear implants and their vocabulary and speech-production growth: is there an added value for early implantation? Ear Hear 2006;27:628–44.


8. Yoshinaga-Itano C, Sedey AL, Wiggin M, Mason CA. Language outcomes improved through early hearing detection and earlier cochlear implantation. Otol Neurotol 2018;39:1256–63.


9. Krishnan LA. Universal newborn hearing screening follow-up: a university clinic perspective. Am J Audiol 2009;18:89–98.


10. Rout N, Parveen S, Chattopadhyay D, Kishore MT. Risk factors of hearing impairment in Indian children: a retrospective case-file study. Int J Rehabil Res 2008;31:293–6.


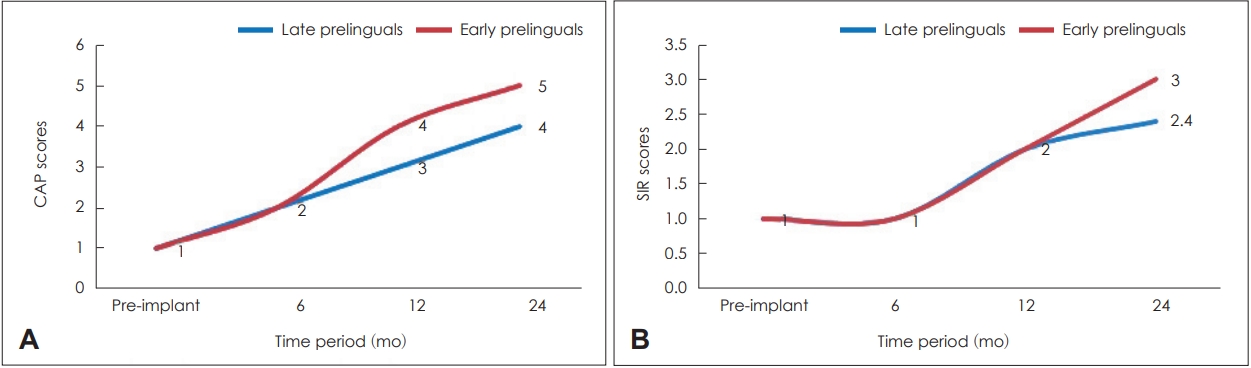
11. Panda S, Sikka K, Singh V, Agarwal S, Kumar R, Thakar A, et al. Comprehensive analysis of factors leading to poor performance in prelingual cochlear implant recipients. Otol Neurotol 2019;40:754–60.


12. Schramm D, Fitzpatrick E, Séguin C. Cochlear implantation for adolescents and adults with prelinguistic deafness. Otol Neurotol 2002;23:698–703.


14. Saleem SM. Modified Kuppuswamy socioeconomic scale updated for the year 2019. Indian J Forensic Community Med 2019;6:1–3.

15. Waltzman SB, Cohen NL. Cochlear implantation in children younger than 2 years old. Am J Otol 1998;19:158–62.

16. Waltzman SB, Fisher SG, Niparko JK, Cohen NL. Predictors of postoperative performance with cochlear implants. Ann Otol Rhinol Laryngol Suppl 1995;165:15–8.

17. Waltzman SB, Cohen NL, Gomolin RH, Green JE, Shapiro WH, Hoffman RA, et al. Open-set speech perception in congenitally deaf children using cochlear implants. Am J Otol 1997;18:342–9.

18. Marazita ML, Ploughman LM, Rawlings B, Remington E, Arnos KS, Nance WE. Genetic epidemiological studies of early-onset deafness in the U.S. school-age population. Am J Med Genet 1993;46:486–91.


19. Smith RJ, Bale JF Jr, White KR. Sensorineural hearing loss in children. Lancet 2005;365:879–90.


20. Grosse SD, Ross DS, Dollard SC. Congenital cytomegalovirus (CMV) infection as a cause of permanent bilateral hearing loss: a quantitative assessment. J Clin Virol 2008;41:57–62.


21. Merugumala SV, Pothula V, Cooper M. Barriers to timely diagnosis and treatment for children with hearing impairment in a southern Indian city: a qualitative study of parents and clinic staff. Int J Audiol 2017;56:733–9.


22. Fang HY, Ko HC, Wang NM, Fang TJ, Chao WC, Tsou YT, et al. Auditory performance and speech intelligibility of Mandarin-speaking children implanted before age 5. Int J Pediatr Otorhinolaryngol 2014;78:799–803.


23. Wheeler A, Archbold SM, Hardie T, Watson LM. Children with cochlear implants: the communication journey. Cochlear Implants Int 2009;10:41–62.


25. Kos MI, Deriaz M, Guyot JP, Pelizzone M. What can be expected from a late cochlear implantation? Int J Pediatr Otorhinolaryngol 2009;73:189–93.


26. Liu R, Jiao Q, Ji F, Wang Q, Zhao H, Li J, et al. The use of the MUSS and the SIR scale in late-implanted prelingually deafened adolescents and adults as a subjective evaluation. Acta Otolaryngol 2020;140:94–8.