Feasibility of Speech Testing Using Wireless Connection in Single-Sided Cochlear Implant Users
Article information
Abstract
Background and Objectives
The speech tests used to evaluate language performance in patients with bilateral deafness (BiD) and cochlear implant (CI) are problematic if applied to patients with single-sided deafness (SSD) because normal ear hearing should be excluded. Thus, we investigated the feasibility of using wireless connection to evaluate speech intelligibility of the CI ear in patients with SSD.
Subjects and Methods
Patients with BiD and SSD were administered the word recognition scores (WRS) and speech intelligibility tests using an iPad-based wireless connection and conventional methods. To exclude normal side hearing in patients with SSD, masking noise and “plugged and muffed” method were used in the WRS and speech intelligibility tests, respectively.
Results
In patients with BiD, the WRS and speech intelligibility tests results using wireless connection and conventional methods were similar. In patients with SSD, the WRS using masking noise in the normal hearing ear was similar to that of using wireless connection. However, 3 of 11 patients with SSD showed under-masked results if using the “plugged and muffed” method.
Conclusions
Speech intelligibility testing using wireless connection is a convenient and reliable method for evaluating CI performance in patients with SSD. The “plugged and muffed” method is not recommended for evaluating CI performance in patients with SSD.
Introduction
Single-sided deaf (SSD) patients experience difficulties with speech recognition in noisy environment and sound localization. SSD occurs in 12–27 per 100,000 individuals, and is usually due to idiopathic sudden sensorineural hearing loss [1]. Cochlear implant (CI) can be a good treatment option for these patients and is supported by considerable evidence [2-4]. The hearing in noise capability of SSD patients significantly improves by using CI compared to that obtained with the contralateral routing of signal or bone-anchored hearing aid [2].
The effectiveness of CI in SSD patients is usually evaluated using the hearing in noise test (HINT); in this test, decreased signal to noise ratio implies that the patients achieved improvements in binaural summation and squelch effect [5]. Indeed, HINT is a very important test for assessing the symptoms of hearing difficulties in SSD patients. Conversely, the speech tests used in bilateral deaf (BiD) patients with CI to evaluate language performance are problematic when applied to SSD patients. To exclude the normal hearing ear, researchers use a masking noise or the “plugged and muffed” method [6-9]. These methods are effective, but they are time- and labor-consuming and require specific environments and devices. More importantly, the normal hearing ear is always a possible confounding factor, as over- and under-masking issues are present when using masking noise and the “plugged and muffed” method, respectively.
Consequently, we used a wireless connection to the CI in SSD patients to perform speech tests. The recorded words or sentences were directly transmitted to the CI device via a wireless connection, thus completely excluding the normal hearing ear during the speech test. We hypothesized that this method would allow reliable evaluation of speech intelligibility in SSD patients after CI surgery. The BiD group result with the conventional method was compared to that with the test with the wireless connection to investigate the reliability of the novel testing method. Then, the SSD group results were analyzed to validate the conventional method using masking noise or the “plugged and muffed” method.
Subjects and Methods
Patients
Retrospectively enrolled in the study were patients who visited our institution after CI for follow-up speech audiogram and speech intelligibility tests between January 1, 2021, and June 1, 2022. The patients concurrently underwent wireless connection testing as well as conventional auditory tests as a clinical routine. A total of 23 patients were enrolled; of these, 15 SSD patients (mean pure-tone threshold at 0.5, 1, 2, 3 kHz for better ear <50 dB) who underwent unilateral CI constituted the SSD group, and 8 BiD patients (mean pure-tone threshold at 0.5, 1, 2, 3 kHz for better ear >70 dB) with unilateral CI served as the control group (BiD group). The Severance Hospital (Seoul, Korea) Institutional Review Board approved this study (project number 1-2021-0044). Informed consent was waived because of the retrospective nature of the study.
Conventional auditory tests
Auditory performances were evaluated before surgery, and annually as possible after switching on of the device. During the follow-up period after operation, aided pure-tone audiometry and speech audiometry were performed in the sound field in the soundproof booth. The sound field consisted of two loudspeakers located at a distance of 1 m and at ±45° from the subject’s head. In SSD patients, a masking noise was applied to the normal hearing ear during pure-tone audiometry and speech audiometry using a headphone. The masking noise was 40 dB louder than the average pure-tone threshold of 500, 1000, 2000, and 4000 Hz in the normal hearing ear. The word recognition score (WRS) was assessed during speech audiometry, using 50 phonetically balanced monosyllabic words at the most comfortable loudness level [10]. Eight of 15 SSD patients and all the BiD patients conducted the speech audiometry test.
To assess speech intelligibility, Categories of Auditory Performance (CAP) score, consonant discrimination, vowel discrimination, mono/disyllabic words (MSW/DSW), and sentence perception tests under auditory-only listening conditions were performed. The tests were performed with samples of words or sentences (modified SNUH Speech Perception Test) in a noiseless room environment at a 65 dB stimulation level, with the sample words or phrases pronounced by a single audiologist positioned 1 m away. All of BiD patients conducted the speech intelligibility tests twice with the conventional method and with a wireless connection. For 11 of 15 SSD patients, a speech intelligibility test was conducted twice with the “plugged and muffed” and wireless connection methods.
Speech tests using wireless connection
The enrolled patients had two different implanted devices: MedEL (Innsbruck, Austria) and Cochlear (Sydney, Australia). In the case of the Med-EL device, a neck loop receiver was needed to connect to the CI device. We used the Bluetooth function on an iPad to transmit the recorded sound signal from the iPad to the speech processor. After connection, the audiologist determined the most comfortable volume level of the device. The WRS was assessed in the most comfortable volume level, using the recorded 50 phonetically balanced monosyllabic words used in conventional speech audiometry in the soundproof booth. As there are currently no validated iPad-based Korean-language words for the speech perception tests, the same set of words/sentences used in the conventional tests were used for this assessment.
Statistical analysis
The Wilcoxon signed rank test was used to compare the conventional method and the wireless connection method in the same group. Statistical analyses were conducted using SPSS 25.0 (IBM Corp., Armonk, NY, USA) and visualized using PRISM 8.0 (GraphPad Software, San Diego, CA, USA). A p-value <0.05 was considered statistically significant.
Result
Results of wireless connection tests in the BiD group
To evaluate the reliability of the speech test using wireless connection, we first compared the test results of the BiD group using the conventional test method with those using the wireless connection (Table 1 and Fig. 1). Because BiD groups have no bias due to contralateral ear in tests, the test results of the two methods should be similar if the wireless method is comparable to the conventional method. The WRS in the sound field in the soundproof booth was similar to that in the test using a wireless connection. The maximal difference was 12% between the two methods. In speech intelligibility test, the maximal differences between the two methods were 10%, 10%, and 4% in MSW, DSW, and sentence, respectively. There were no significant differences in the result of the two methods when using pairwise statistical analysis. These results support that the wireless method is comparable to the conventional method.
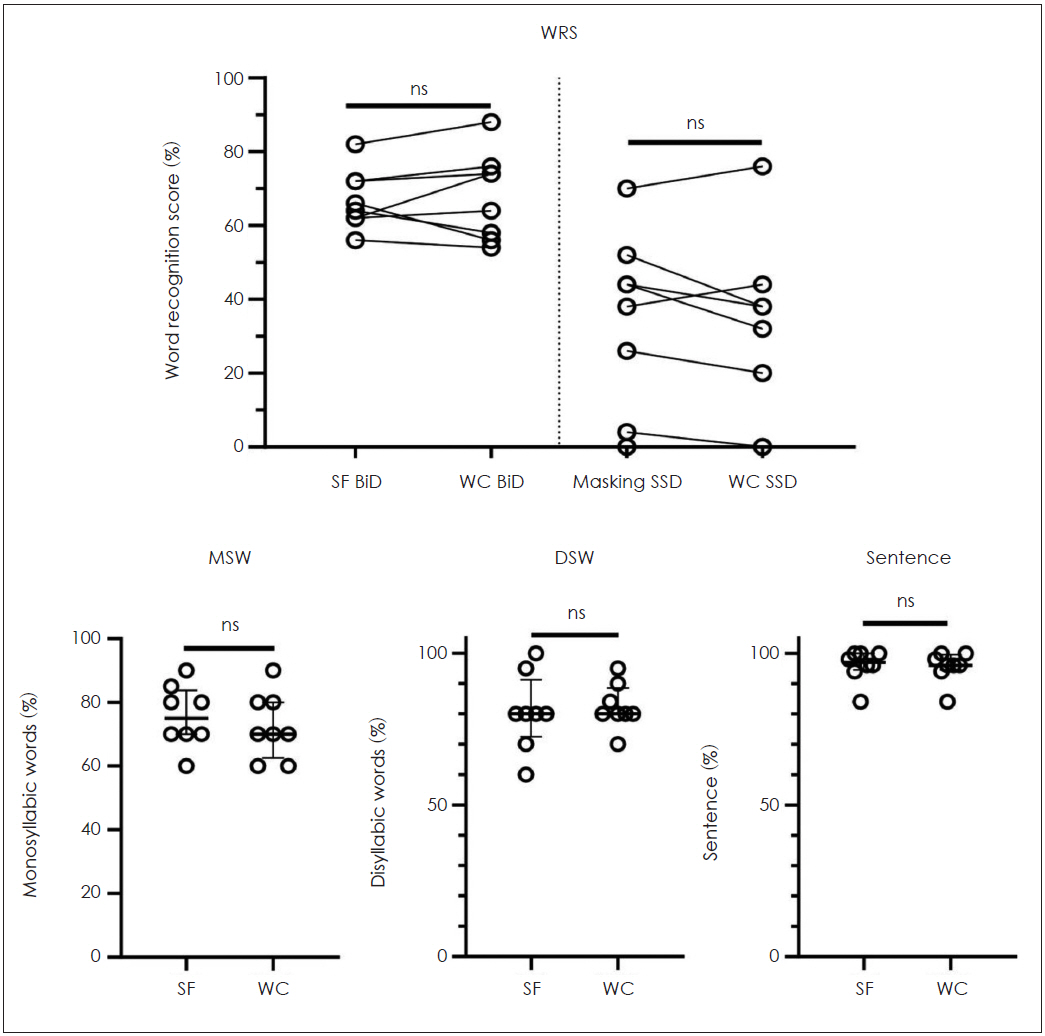
Word recognition score results of all groups (upper) and speech intelligibility test results of BiD patients (lower). In the graphs on the bottom, the median (thick line) and interquartile range (thin error bar) are marked. n=8 in both group. WRS: word recognition score, SF: sound field, BiD, bilateral deafness; SSD, single-side deafness; WC, wireless connection; ns, not significant; MSW, monosyllabic words; DSW, disyllabic words.
Results of wireless connection tests in the SSD group
Next, we evaluated the WRS of the SSD group by applying the masking noise to the normal hearing ear. The result was similar to that using a wireless connection. The maximal difference between the two methods was 14%. There was no statistically significant difference between the methods when using pairwise analysis. These results suggested that the masking noise in the soundproof booth was effective in inhibiting the normal hearing ear in the SSD group.
However, there are noticeable different results between the two methods when they were applied to speech intelligibility tests. The speech intelligibility test was conducted using two different methods (“plugged and muffed” and wireless connection) in SSD patients. The results showed statistically significant differences in several categories (Fig. 2). Specifically, CAP score (p=0.031), vowel discrimination (p=0.012), and MSW (p=0.031) were significantly poorer when using a wireless connection. In addition, there were three patients who showed a large gap of more than 10% in sentence scores. Their sentence scores were 38%, 100%, and 88%, respectively in conventional test with plugged and muffed method. However, in wireless connection test, their sentence scores were under 10%. Given that their speech intelligibility results using a wireless connection were commonly poor in all subtests compared with those in the “plugged and muffed” method, an under-masked result was suspected.
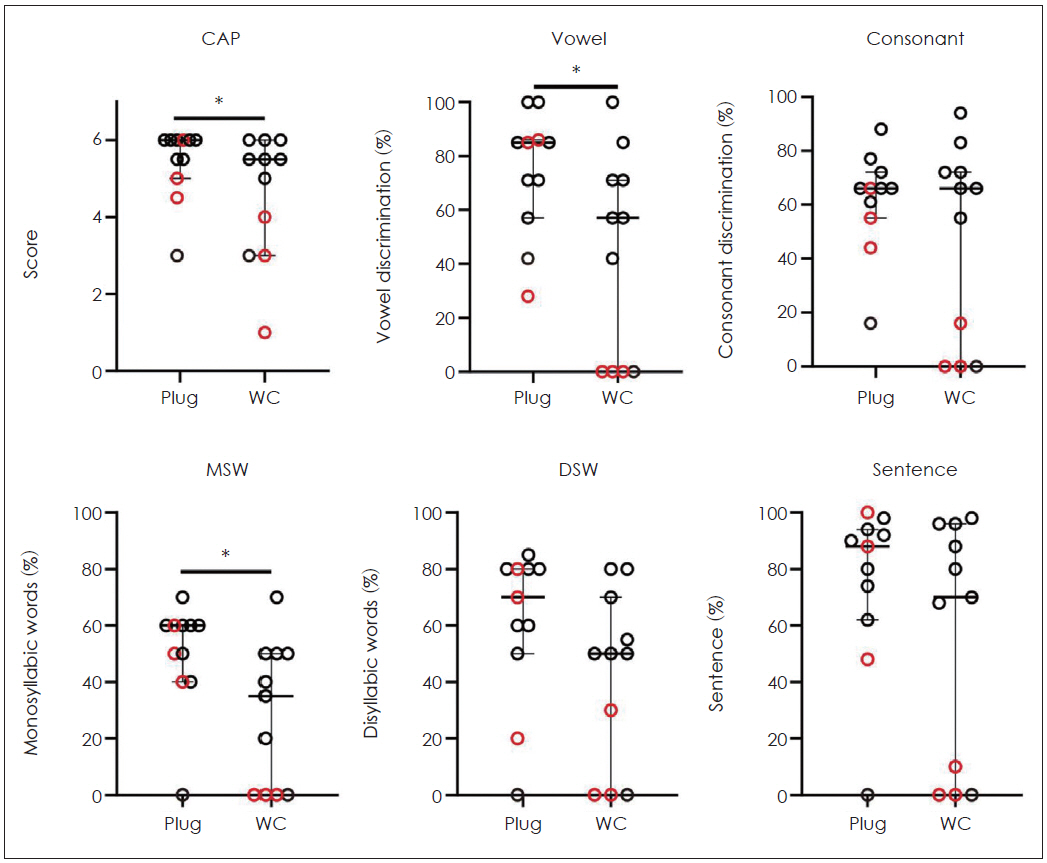
Speech intelligibility of the single-sided deafness group (n=11) with the “plugged and muffed” method and a wireless connection. The red hollow circles indicate the subjects who showed more than a 10% difference in sentence score between the two methods. *p<0.05. CAP, categories of auditory performance; Vowel, vowel discrimination; Consonant, consonant discrimination; MSW, monosyllabic words; DSW, disyllabic words; Plug, plugged and muffed method; WC, wireless connection; ns, not significant.
Discussion
Our study proved that speech tests using a wireless connection to CI devices have an advantage in the prevention of under-masking compared to the “plugged and muffed” method. In the BiD group, there was no significant difference in test results between the conventional methods and the wireless connection. Similarly, there were no differences between the two methods in the SSD group upon applying the masking noise in the normal hearing ear. However, the speech intelligibility test for SSD patients using the “plugged and muffed” method showed significantly better results which are suspected of under-masking in several categories compared with the wireless connection method (Fig. 3).

The graphical summary of this study. Blue arrows indicate similar results between the two methods. Red arrows indicate significant different result between the two methods. WRS, word recognition score using conventional method; Wireless WRS, word recognition score using wireless connection method; SIT, speech intelligibility tests; Wireless SIT, speech intelligibility tests using wireless connection method.
The wireless connection to the CI device is intended to help patients hear the directly transmitted signal from electronic devices such as the telephone or television. With the development of smartphones and their applications, wireless connection has become more widely applied to CI patients. We tried this method to evaluate CI patients’ speech intelligibility, and to determine the exact function of the implanted ear while excluding the normal ear. As the exclusion of a contralateral side hearing was de facto in the BiD group, the results should be similar between the two methods if the speech test using a wireless connection was accurate. Indeed, given the similar results for the BiD group among the conventional method and the wireless connection, the WRS and speech intelligibility test using the wireless connection seem reliable.
Applying masking noise to the normal hearing ear seems effective, given that the WRS of the SSD group showed similar results regardless of the method used. However, the “plugged and muffed” method showed under-masked results in 3 of 11 SSD patients. Although the number of subjects was too small to identify statistically significant risk factors for the under-masking, the under-masked subjects showed poor CI speech intelligibility in common. Residual hearing did not cause the under-masking because the three under-masked subjects were deaf in the operated ear. The “plugged and muffed” method can attenuate 44–66 dB of sound [11]. Given our results, this method does not provide a consistent degree of sound attenuation. Therefore, although it is easier than applying masking noise, the “plugged and muffed” method is not recommended in SSD patients.
Compared with the conventional method, wireless connection seems to be a simple and reliable method to inhibit the normal hearing ear. Meanwhile, several groups have tried directly connected audiometric testing via electrical cable connection [4,12,13]. The direct connection system is expected to be equivalent to the wireless connection in inhibiting the normal hearing ear. Yet, to the best of our knowledge, the feasibility of speech testing using wireless connection had not been tested prior to this study. With the advancement of technology, wireless connections are projected to replace electrical cables in the near future. Thus, we expect the result of this study can support the rationale for speech tests using a wireless connection.
This study has some limitations. Mainly, there are no validated iPad-based Korean-language words for the speech perception tests. In the future, such tests should be developed and validated not only for hearing-impaired patients but also for the general population, similar to the existing English and Japanese versions [14,15]. In addition, this study is not including sound localization and hearing function in noise which are major functional advantages of CI in SSD. Future studies with these tests can suggest concrete evidence of the advantage of the wireless connection method compared to the “plugged and muffed” method.
In conclusion, speech intelligibility testing using a wireless connection is a convenient and reliable method for evaluating CI performance in SSD patients. In addition, the “plugged and muffed” method is not recommended for evaluating CI performance in SSD patients because of this technique’s high rate of under-masking.
Acknowledgements
This study was supported by a faculty research grant of Yonsei University College of Medicine for 6-2018-0086 (granted to J. Y. Choi). This work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIP) (2020R1A2C3005787).
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Jae Young Choi. Data curation: Ji Hye Hur, Youngrak Jung, Jeong Ha Kim. Formal analysis: Seong Hoon Bae. Funding acquisition: Seong Hoon Bae. Methodology: Seong Hoon Bae. Project administration: Youngrak Jung. Visualization: Seong Hoon Bae. Writing— original draft: Jae Young Choi, Seong Hoon Bae. Writing—review & editing: Jae Young Choi, Seong Hoon Bae. Approval of final manuscript: all authors.

