Two Cases of Multiple Ossicular Chain Disruption After Penetrating Injury and Tympanic Membrane Healing
Article information
Abstract
Ossicular chain disruption is a typical consequence of temporal bone trauma. However, it can also occur as a result of direct trauma to the ossicular chain due to penetrating injuries. Hearing loss, dizziness, and facial nerve damage could also occur after penetrating middle ear injuries. Multiple ossicular chain disruption is a rare traumatic ossicular complication caused by direct penetrating lesions in the external auditory canal. We present two cases of multiple ossicular disruptions (dislocation of the incudostapedial and malleoincudal joints) after ear-pick injuries, both of which resulted in conductive hearing loss. The condition improved after delayed surgical intervention (ossiculoplasty).
Introduction
Ossicular chain injury is a frequent complication of temporal bone fracture and penetrating injury through the external auditory meatus. Temporal bone fractures and injuries that penetrate the external auditory meatus frequently result in ossicular chain damage [1].
Traumatic ossicular injuries can be categorized into: incudostapedial (IS) separation, malleoincudal (MI) separation or dislocation, dislocation of the malleus or incus, stapediovestibular dislocation, and fracture of the ossicles [2]. Depending on the type and location of the ossicular injury, conductive, sensorineural, or mixed hearing loss can be observed. Other symptoms, such as vertigo, nausea, and tinnitus may also occur [1].
Trauma to the temporal bone with or without fracture remains the predominant cause of ossicular injury, while ossicular injuries from ear picks are rare [3]. However, of the injuries caused by foreign body insertion, the most common is ear-pick injury. Even years after the event, conductive hearing loss caused by ossicular injury typically improves with surgical treatment [4].
Here, we report two cases of multiple ossicular chain disruption caused by penetrating injury that presented with conductive hearing loss that improved after surgery.
Case Report
Case 1
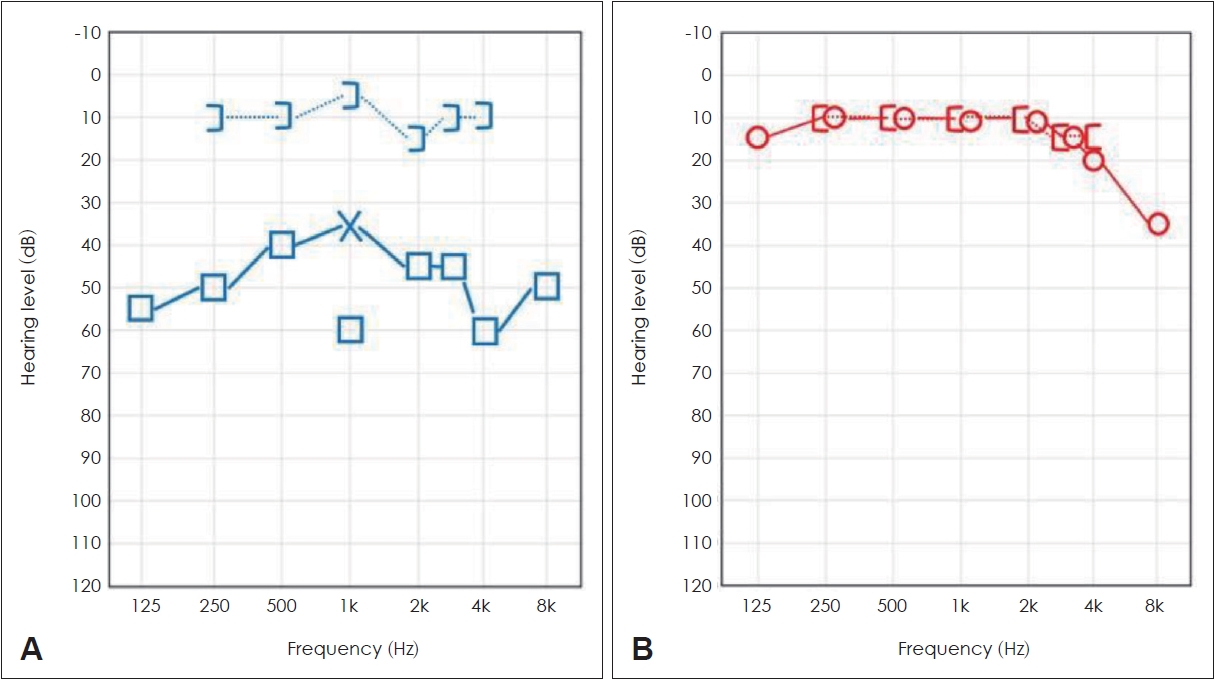
A 17-year-old male patient presented to our ENT department with the chief complaint of hearing loss on the left side. The patient had a history of being stabbed with an ear pick through the left ear canal by his older brother in childhood, which led to hearing loss. Although hearing loss occurred shortly after the accident, no further evaluation or management was performed at that time. During the physical examination, we found an intact tympanic membrane (TM) with no abnormal findings (Fig. 1A). However, pure-tone audiometry (PTA) showed conductive hearing loss with a 48-dB air-bone gap in the left ear (Fig. 2A). Temporal bone computed tomography (TBCT) revealed partial ossicular destruction; hence, explorative tympanotomy and ossiculoplasty were performed (Fig. 3A and B). Surgical findings revealed dislocation of the IS and MI joints, fracture of the supra-structure of the stapes, and that the stapes was tilted forward. The suprastructure of the stapes was removed, and the hypomobility of the footplate and round window reflex were assessed (Fig. 4A). A total ossicular replacement prosthesis (5.0-mm-length, titanium) was placed after removal of the suprastructure of the stapes (Fig. 4B). During recovery, bed rest with head elevation and antibiotic administration were prescribed. At the 3-month follow-up, we performed PTA to confirm progress. Although it showed an improvement in air conduction hearing from 63 dB to 41 dB, the air bone gap remained (Fig. 5A). We recommended CT follow-up to identify the cause, but the patient was lost to follow-up. We suspect that the raised prosthesis may have been fixed backwards or detached from its position.
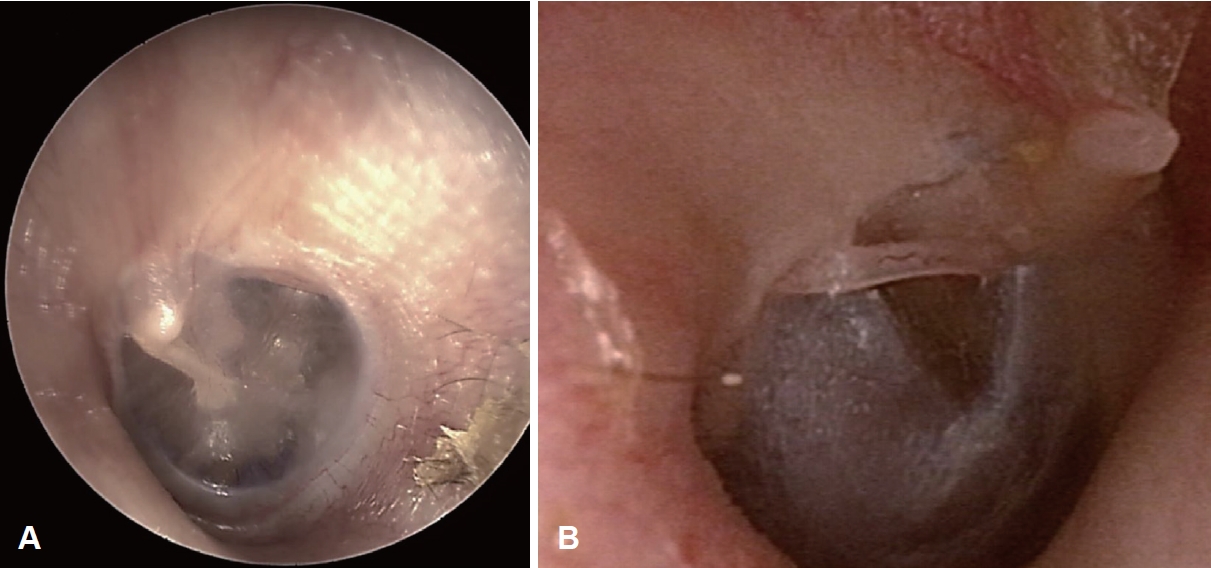
Otoscopic findings. A: The left tympanic membrane of Case 1. B: The right tympanic membrane of Case 2. The malleus is protruding into the external auditory canal.
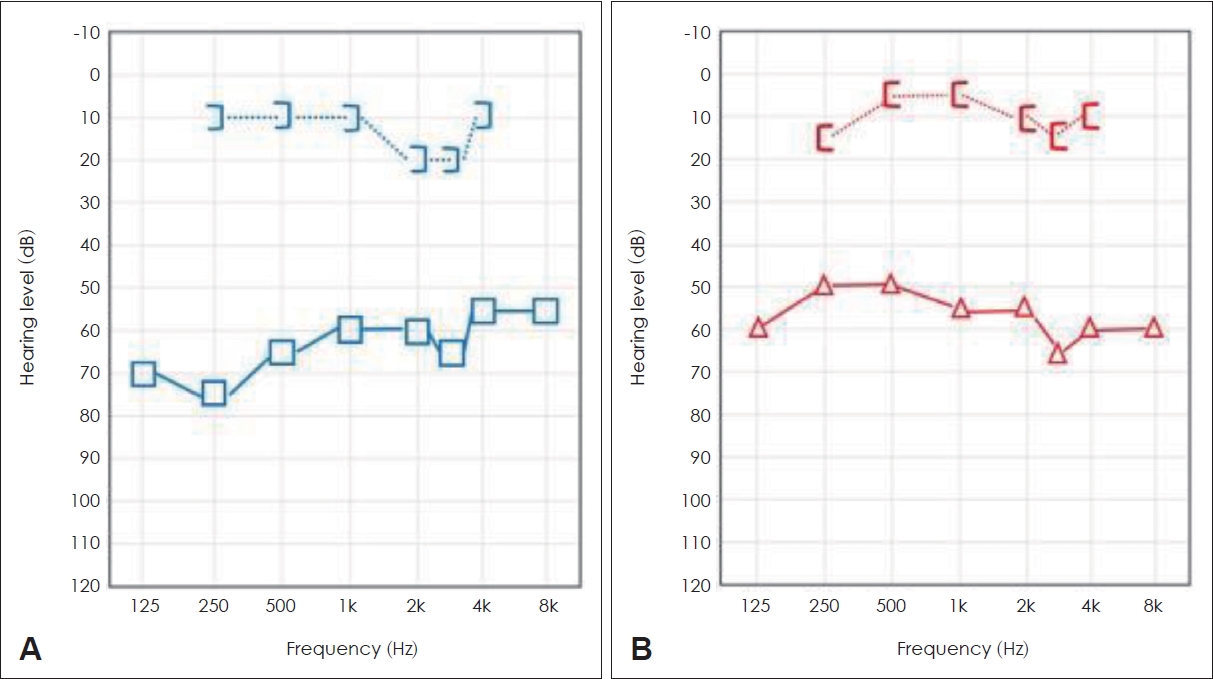
Preoperative audiograms showing conductive hearing loss with an air-bone gap. A: Left ear of Case 1. B: Right ear of Case 2.

Preoperative axial temporal bone CT. A: Slight dislocation of the malleoincudal (MI) joint axis (yellow arrow) in Case 1. B: Stapes is faintly identified (yellow arrow) in Case 1. C: Dislocated right MI joint (yellow arrow) in Case 2. D: Malleus handle (red arrow) protruding into the external auditory canal in Case 2.
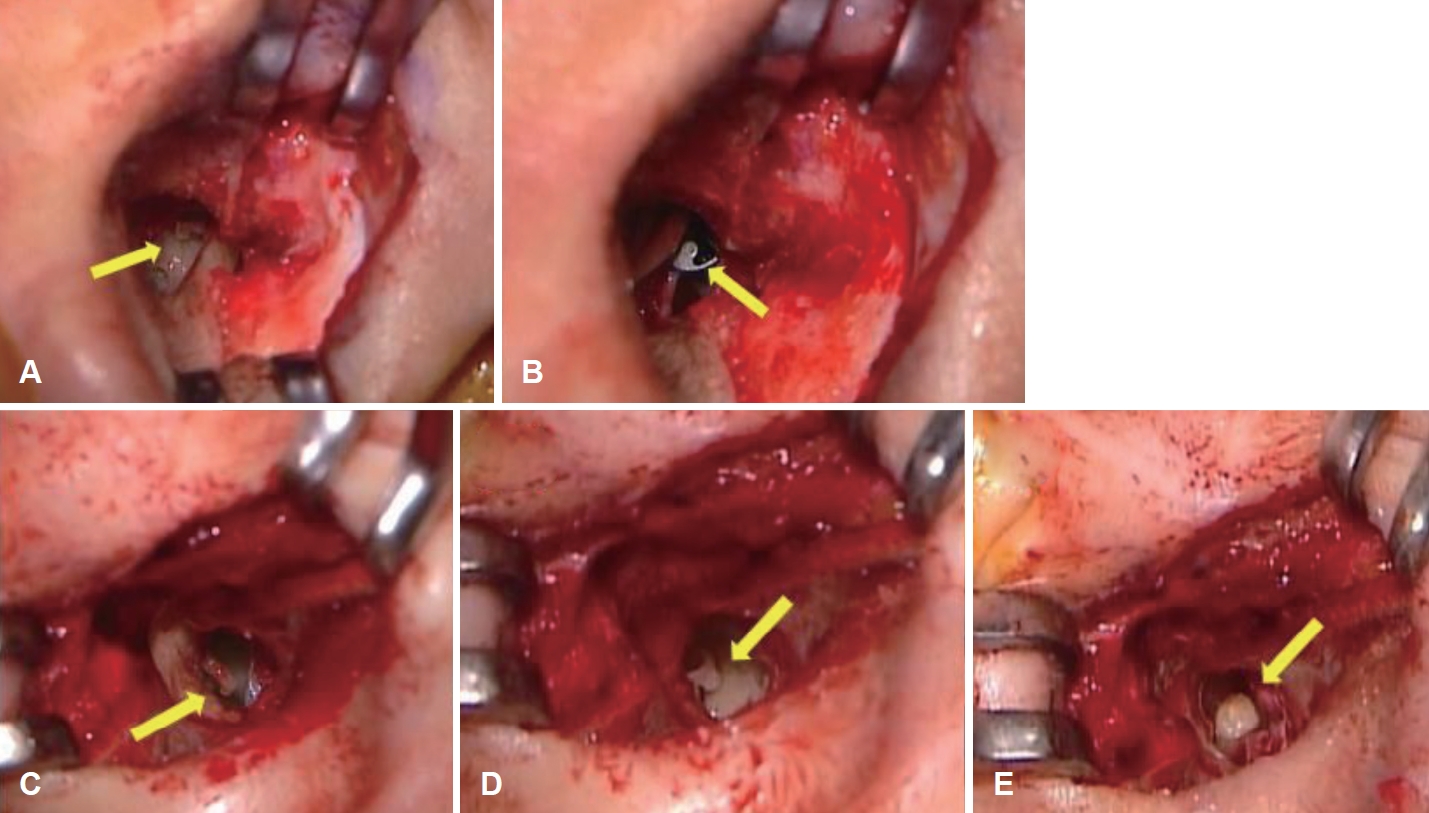
Intraoperative findings of the patients. A: Dislocation of the incudostapedial (IS) joint (yellow arrow) in Case 1. B: After prosthesis (yellow arrow) insertion in Case 1. C: Dislocation of the IS joint (yellow arrow) in Case 2. D: Stapes (yellow arrow) is slightly lying down in Case 2. E: After incus collumelization (yellow arrow) in Case 2.
Case 2
A 40-year-old female patient visited our ENT department with right-sided hearing loss. The patient has a history of left ear perforation that occurred while cleaning it with an ear pick. In addition, the patient had a history of chronic external otitis in both ears accompanied by tinnitus. On physical examination, a dislocation of the malleus handle to the superoposterior portion of the TM was observed in the left eardrum (Fig. 1B). PTA revealed conductive hearing loss with a 48-dB air-bone gap in the right ear (Fig. 2B). TBCT showed dislocation of the IS and MI joints, and the malleus handle protruding toward the external auditory canal of the right ear (Fig. 3C and D). Explorative tympanotomy was performed, and the malleus handle was generally dislocated and attached to the anterior end of the TM. Dislocations of the IS joint, MI joint, and stapes were slightly laid down (Fig. 4C and D). The malleus and incus were removed, and short collumelization was performed with the autologous incus (Fig 4E). The surgery was completed after tympanoplasty using the tragal cartilage. Following surgery, conservative therapy, including bed stabilization with head elevation and antibiotic administration, was prescribed. The patient’s hearing improved, and had recovered to normal at the 3-month follow-up after surgery (Fig. 5B).
Discussion
Head trauma is the most common cause of ectopic dislocation, and analysis of the resulting pattern of ectopic dislocation has been conducted in several studies. However, it is rarely caused by direct trauma to the ear bone. Domestic incidents of ear bone dislocation from trauma are extremely uncommon, and the majority of such cases are reported by other countries, particularly Japan, due to the popularity of certain ear cleaning procedures [4,5].
There were two distinct aspects of our case reports. First, the patients showed multiple ossicular chain disruptions, which are very rare penetrating injuries typically caused by ear picks. Second, the patients recovered after surgical therapy, even when the surgery was performed long after the trauma.
Among several types of ossicular injuries, IS dislocation is the most frequent ossicular chain disruption following head trauma [6-8]. The malleus and stapes are more resistant to disarticulation or severe injuries than the incus. The malleus is the ossicle that is more firmly attached, and the TM, tensor tympani tendon, and anterior and lateral mallear ligaments anchor it [7]. The MI joint is additionally shielded within the epitympanic recess [6,9]. In our cases, the two joints were damaged by penetrating injuries, but there was no damage to the inner ear because the footplate was preserved.
When determining whether there has been traumatic ossicular disruption, high-resolution TBCT is crucial in identifying any loss of normal ossicular articulation [10,11]. The diagnosis in our cases was confirmed by TBCT findings, which also helped to confirm the dislocation of ossicles during surgery. The decision regarding ossicular reconstruction of conductive hearing with the autologous incus, partial ossicular replacement prosthesis, or total ossicular replacement prosthesis depends on the type and location of injury to the ossicular chain [8,12].
In conclusion, our cases involved long-standing multiple ossicular chain disruption resulting from penetrating injuries treated with surgery that yielded satisfactory hearing outcomes. Therefore, ossicular bone dislocation should be investigated if hearing loss does not improve following hemotympanium absorption or eardrum perforation repair [4]. Following trauma, ossicular reconstruction results in more stable and better hearing outcomes, even in cases of delayed treatment [4].
Acknowledgments
This research was supported by a fund from the Biomedical Research Institute at Jeonbuk National University Hospital. We would like to acknowledge the Research Institute for Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital for supporting this study.
Notes
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee. Written informed consent was obtained from the patients for their anonymized information to be published in this article.
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Eun Jung Lee, Cha Dong Yeo. Formal analysis: Eun Jung Lee, Cha Dong Yeo. Project administration: Cha Dong Yeo. Supervision: Eun Jung Lee, Cha Dong Yeo. Visualization: Cha Dong Yeo. Writing—original draft: Sola Han. Writing—review & editing: Sola Han. Approval of final manuscript: all authors.