A Case of Post-Traumatic Meniere's Disease
Article information
Abstract
There are only a few reports of post-traumatic Meniere's disease and there is few literature that contains detailed data associated with the disease. We report a case of post-traumatic Meniere's disease. He suffered from tinnitus, fluctuating sensorineural hearing loss, and recurrent vertigo. Symptomatic medical treatment was not helpful and neither was soft tissue plugging around the oval and round windows during exploratory tympanotomy. Three months after soft tissue plugging, endolymphatic sac decompression surgery was performed. The patient's symptoms improved markedly thereafter. The clinical significance of post-traumatic Meniere's disease is described and we present a brief review of the literature.
Introduction
Post-traumatic Meniere's disease (PTMD) is Meniere's syndrome that develops after acoustic or physical trauma. The histopathologic characteristics of PTMD are identical to those of idiopathic Meniere's disease.1) The causes of traumatic insult that lead to PTMD include blows to the head, temporal bone fractures, previous ear operations such as stapedectomy, or acoustic trauma.2) Since 1952, fewer than 6 articles describing PTMD have been published and little data regarding the management of this disease are available in the literature.1,2,3,4,5,6) We present a case of PTMD patient who suffered from intractable Meniere's disease symptoms and showed improvement after endolymphatic sac decompression (ELSD).
Case Report
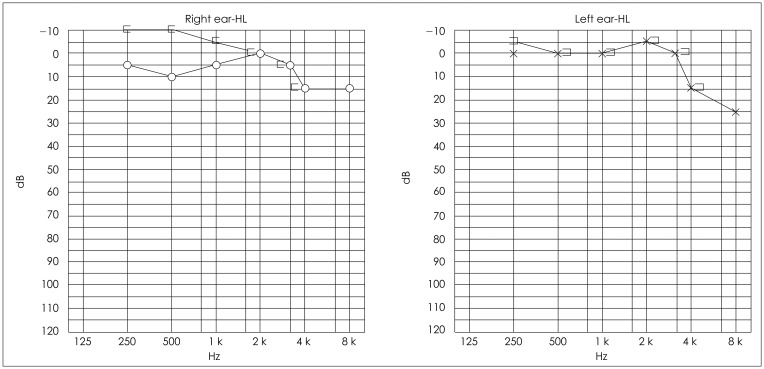
A 31-year-old man was referred to our otology clinic with right tinnitus, ipsilateral aural fullness, and recurrent vertigo over 2-month following a car accident. The patient had no other complaints, such as otalgia or facial weakness. Both tympanic membranes were normal. His hearing was normal on the day of admission; however, at second day after admission, pure tone audiometry showed a 25-dB threshold shift at low frequencies on the right side (Fig. 1). Hearing on the patient's right side had a fluctuating pattern and he reported recurrent vertigo after aggravation of aural fullness-the symptoms of endolymphatic hydrops. Temporal bone high-resolution CT and brain magnetic resonance imaging revealed no evidence of a specific lesion or abnormality. The results of a caloric test, electrocochleography, and a vestibular evoked myogenic potential test were normal and video nystagmography showed a left-beating nystagmus in all position. The patient was diagnosed with PTMD and we began to treat him with diuretics, systemic/intratympanic steroid therapy, and vestibular suppressants. After 4 months of medical treatment, he suffered from persistent tinnitus, fluctuating right sensorineural hearing loss, and severe recurrent vertigo with left-beating nystagmus.
Pure tone audiogram results at admission (A) and second day after admission (B). Low tone sensorineural hearing loss was observed in the right ear at second day after admission.
To rule out perilymphatic fistula, an exploratory tympanotomy was performed 4 months after medical treatment began. Although no perilymph leaks were observed, the oval window and round window were obliterated with soft tissue to ensure that any unobserved perilymph leaks were plugged. After surgery, the patient's symptoms had shown no improvement. ELSD was performed for the reduction of his symptoms 2 months later.
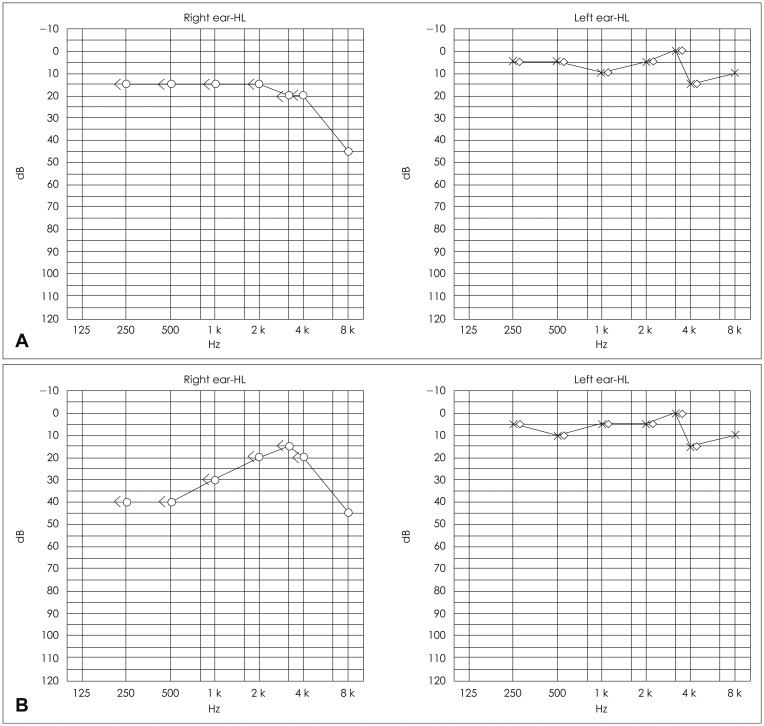
The patient did not complain of any vertigo in the month following ELSD, and he did not take any medication to control dizziness. Although his tinnitus was persistent, his hearing was within normal limits and ear fullness disappeared (Fig. 2). Pure tone audiometry showed some air-bone gap at low frequency on right side, but re-evaluation after the operation did not show any reason. However, after 1 month, mild dizziness started to recur and medical treatment for Meniere's disease was resumed. The frequency and severity of his dizziness (not vertigo) were reported to be less than half of what he had experienced before surgery. We used the Dizziness Handicap Inventory (DHI) scale to compare vertigo attacks before and after treatment. DHI scale decreased from 84 preoperatively to 16 after 6 month (Table 1).
The patient has been undergoing regular follow-up care, and has not experienced aggravation of his symptoms in the year following ELSD.
Discussion
Up to recently, otorhinolaryngologists were not familiar with PTMD. Although PTMD seems to be very rare, it is an important clinical entity with respect to the results of clinical and histopathologic studies.2) The causes of traumatic endolymphatic hydrops (identical to PTMD) are presumed to involve an increase in the volume of endolymph in the cochlear duct after traumatic damage to the labyrinth. The causative mechanisms suggested in previous studies include the following: fistulization of the bony labyrinth that may cause a disturbance of the perilymph-endolymph pressure homeostasis; direct injury to the membranous labyrinth that may induce an increase of lymphatic fluid in the cochlear duct due to irritation of the membranous labyrinth; and damage to the endolymph drainage system due to temporal bone fracture or iatrogenic injury to the saccule.5) Fissures from the temporal bone may extend through the vestibular aqueduct, causing fibro-osseous blockage of the endolymphatic duct, and iatrogenic injury to the saccule may obstruct the longitudinal flow of endolymph. Additionally, trauma may induce dysfunction in cells producing or absorbing endolymph. Therefore, trauma may lead to dysfunction in endolymphatic passage, production, or absorption. Impulse trauma to the membranous labyrinth may also displace the epithelia of sensory end organs or other cellular elements such as the otoconia of the saccule or utricle.1) The resulting floating cellular debris may cause a disturbance of endolymph absorption through the endolymphatic duct, either mechanically or chemically, and lead to endolymphatic hydrops. Finally, direct or indirect injury of the endolymphatic duct or sac as a result of traumatic insult may induce blockage of the endolymphatic drainage system. On the other hand, perilymphatic fistula can induce an imbalance between perilymphatic and endolymphatic pressures. If leakage of perilymph continues, the perilymphatic pressure drops, leading to endolymphatic hydrops.5) In our case, exploratory tympanotomy was performed to exclude the possibility of perilymphatic fistula, and no lesions indicative of fistula were found.
The clinical manifestations of PTMD may be different from those of typical Meniere's disease. One of these differences is a delay in the onset of symptoms. In PTMD, symptoms do not usually develop for several years after the traumatic event.2) Some researchers have concluded that all patients who experience acoustic trauma show symptoms of Meniere's syndrome one or more years (up to 20 years) after the trauma; however, approximately one-third of patients with physical trauma develop Meniere's syndrome within 1 month after trauma.1) Further, these researchers suggest that it may become more difficult to speculate about causative relationships as the time between trauma and the onset of Meniere's syndrome increases. In our case, the patient first began experiencing symptoms within 2 months after car accident, which may indicate an early-onset type of endolymphatic hydrops.
Direct injury to the membranous labyrinth results in endolymphatic hydrops that may not be progressive and that subsides soon after injury, leaving high-tone hearing loss. In contrast, injury to the endolymphatic fluid drainage system may induce endolymphatic hydrops that is delayed in onset and usually persistent.5) If there is definitive evidence of traumatic history in a patient with Meniere's symptoms, the clinician should consider the possibility of PTMD.
PTMD can be managed in accordance with the treatment for Meniere's disease. Severe or rapid head movements are not recommended for patients with these symptoms, and medical treatment can be considered as the first therapeutic option. Vestibular suppressants can be used for patients susceptible to attacks of vertigo. Medical treatment may also include a low-salt diet, betahistine hydrochloride, diuretics, steroids (systemic or intratympanic), and a low-pressure pulse generator (Meniett®, Medtronic Inc., Jacksonville, FL, USA). If medical treatment is not effective, chemical labyrinthectomy, such as intratympanic gentamycin injection, or surgical treatment, such as ELSD, labyrinthectomy, cochleosacculotomy, or vestibular nerve section, can be considered.7)
A previous study reported 3 PTMD cases that developed after stapedectomy.5) Two of the patients in the study were treated by repair of the perilymphatic fistula and 1 patient was treated medically. The patient in the present case did not have a history of iatrogenic trauma and has been able to tolerate his symptoms after ELSD. If the patient's symptoms increase and are persistent, chemical labyrinthectomy, such as with intratympanic gentamycin injection, may be performed considering his hearing.
To evaluate the patient's disability from dizziness before and after treatment, the patient was asked to complete the DHI. The DHI is a questionnaire designed by Jacobson and Newman8) to assess self-perceived handicapping due to dizziness.9) In the present case, as the frequency of vertigo attacks decreased, there was a corresponding decrease in the DHI score. The patient's DHI score did not change after initial medical treatment or exploratory tympanotomy. However, it was markedly reduced until 6 months after ELSD. Although the patient transiently felt mild-to-moderate dizziness 1 month after ELSD, his symptoms were well controlled after resumption of medical therapy, which included diuretics, dimenhydrinate, and vestibular suppressants.
In conclusion, although PTMD is rare and unfamiliar to most clinicians, the possibility of its occurrence should be considered as the frequency of traumatic accidents increases. Prompt and accurate diagnosis and appropriate treatment for PTMD is important for improvement of the patient's quality of life.