Can Wideband Tympanometry Predict the Prognosis of Otitis Media With Effusion?
Article information
Abstract
Background and Objectives
This study aims to evaluate the capacity of wideband tympanometry (WBT) in predicting the prognosis of otitis media with effusion (OME).
Subjects and Methods
Sixty-one ears with effusion and 30 healthy ears of children were enrolled. The patients were followed up monthly using WBT. After the completion of measurements, the ears were separated into four groups according to the duration of recovery; Group 1: Good prognosis (≤1-month, n=18), Group 2: Worse prognosis (>1-month, n=29), Group 3: Surgical (no recovery, n=14), and Group 4: Control (healthy ears, n=30). Tympanometric peak pressure (TPP), resonance frequency (RF), and absorbance levels were compared within and between the groups.
Results
The TPP and RF values of the study group were lower than those of the controls (p<0.001). The ears with OME had lower absorbance measures than the controls at all frequencies; the differences were significant at 250, 500, and 1,000 Hz (p<0.001). However, at 2,000 Hz, the absorbance levels of the ears with OME were similar with those of the control group only in the good prognosis group (p>0.05). The receiver-operating characteristic analysis revealed that absorbance measures over 0.237 and 0.311 at 1,000 Hz and 2,000 Hz, respectively, have sensitivities and specificities over 70% for prediction of good prognosis, and the calculated odd ratio for these measures were 6 (p<0.05).
Conclusions
WBT measurement is promising in predicting the recovery of OME in children.
Introduction
Otitis media with effusion (OME), which is defined as the existence of fluid in the middle ear without pain and fever, causes conductive hearing loss (CHL) [1,2]. It is the most common cause of the preventable hearing loss in developed countries [3]. Approximately 90% of children in preschool age experience OME, which yields to increased costs either direct or indirect by affecting the social and school performance [2,4,5].
Although the diagnosis of OME stands primarily on pneumatic otoscopy; tympanometry should also be performed in children with a suspected OME. Conventional tympanometry, in which 226 Hz stimulus is used as the probe tone, has been one of the most valuable and commonly used tools in audiological assessment of the patients with CHL for decades. However, it is incapable of differential diagnosis of specific problems of ossicular chain, such as discontinuity or fixation. The studies, in which multi-frequency probe tones were used for immittance measurements, show variable absorbance and reflectance properties of different middle ear pathologies [6-9]. Standing on those, it seems that multi-frequency tympanometry has a potential for precise differential diagnosis, which cannot be done by conventional tympanometry. Furthermore, middle ear pathologies caused by Eustachian tube dysfunction, like OME, may be misdiagnosed due to the incapability of conventional tympanometry, especially in infants because of their different acoustic characteristics of the auditory canals, tympanic membranes, and middle ears [10-12]. This phenomenon leaded the usage of 1,000 Hz probe tone tympanometry, which is more precise for the diagnosis of OME, in infants. However, currently there is no tool for helping physicians for the prediction of the prognosis of OME.
A prolonged OME is an important public health issue and may have an effect on a child’s speech and language as well as social development [13,14]. Shortening the period with hearing loss caused by OME would clearly be beneficial and it would be ideal to be able to predict the prognosis of OME with objective measurements. Prediction of the prognosis will be beneficial for individuals suffering OME, as early detection of a patient who is a candidate for surgery would clearly help bypassing the period with CHL. Consequently, the complications caused by hearing loss might be avoided. It would also be beneficial for public health by decreasing the number of hospital visits and overall cost of the disease. We hypothesized that wideband tympanometry (WBT), which automatically uses 250 Hz to 8,000 Hz wideband stimulus for immittance measurement, may be able to help predicting the prognosis of OME. The objective of this study is to investigate the capability of WBT in predicting the prognosis of OME by using objective measures.
Subjects and Methods
After the approval of Erciyes University Clinical Research Ethics Commitee (Nr: 2014/98), 31 patients (61 ears) between the ages of 2-10 who were diagnosed with OME were enrolled into this prospective and controlled cohort study. A written informed consent was received from each patient. All of the children in the study groups had either Type B or Type C (tympanometric peak pressure [TPP] <-50 daPa) tympanograms. The children who had a tympanic membrane retraction, history of any otologic intervention and cranio-maxillofacial anomalies were excluded. The ones who were planned to have adenoid or tonsillar surgery and ventilation tube (VT) insertion at the initial visit were also not enrolled. Fifteen children (30 ears) who had healthy ears including normal examinations as well as normal TPP (between -50 daPa and +50 daPa) were enrolled as a control group [15,16]. Each ear was evaluated separately.
After the initial otoscopic examination, conventional tympanometry (Madsen Zodiac 901, Otometrics, Taastrup, Denmark) and WBT (Titan, Interacoustics, Assens, Denmark) tests were applied to each ear. For the conventional tympanometric measures, a pressure range of -200 to 400 daPa, a pump speed of 200 daPa/s and 226 Hz probe tone were used. For wideband measures, a pressure range of -600 to +300 daPa, and an automated pump speed which starts with high speed (300 daPa/s) and slows down to low pump speed (50 daPa/s) around the peak of the tympanogram were used. TPPs were measured; absorbance values at 250-8,000 Hz frequencies at that pressure level and resonance frequencies (RFs) were recorded. The hearing levels of the children was measured either with a pure tone audiometry or pediatric conditioned play audiometry according to the age but the results were not used for analysis since the measurements were not standard for analysis because of the varying ages of children.
The measures were performed only once in the control group, the ears in the study group were taken to monthly follow-up and the tests were repeated at each visit. If an ear was normal in the examination and have normal tympanometric results during follow-ups, the tests were performed one more time after a month and if the normal results persisted, the ear was dropped from monthly follow-ups. VTs were applied if a detoriation or no improvement was seen in the TPP levels at 3rd month. The follow-up was continued until the 6th month if the TPP levels are improving but still not normal at each measure. If a Type A tympanogram was still not achieved at the 6th month, VT was applied.
After the measures were completed, the ears were separated into four groups (Fig. 1); Group 1: The ones that OME recovered in a month (Good prognosis group), Group 2: The ones that OME recovered in more than a month (Worse prognosis group), Group 3: The ones that VT was applied (Surgical group), Group 4: Healthy ears (Control group).
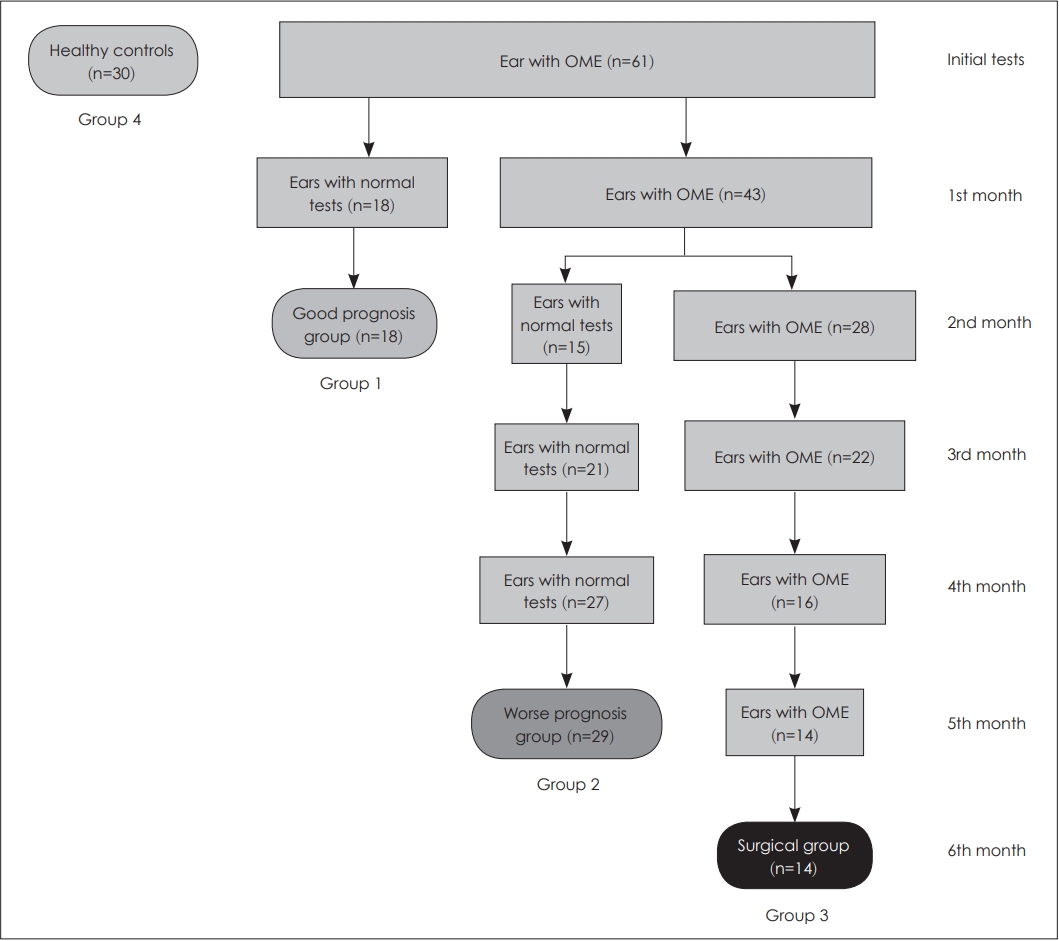
Flowchart demonstrating the method of the study. n, number of ears; OME, otitis media with effusion.
The TPP measures, the absorbance levels of 250, 500, 1,000, 2,000, 4,000 and 8,000 Hz frequencies at the TPP level, and the RF levels of the study groups were compared with control group. The measurements of the study groups were also compared within the groups.
Statistical analysis
Histogram, q-q plots were examined, and Shapiro-Wilk’s test was performed to assess the data normality. Levene test was used to test the variance homogeneity. Friedman and KruskalWallis tests were applied to conduct within-group and between-group comparisons. Bonferroni corrected Dunn’s test was used for multiple comparison analysis. Receiver operating characteristic (ROC) curve analysis were applied to assess the predictive performance of absorbance measures inOME. Area under the ROC curves were calculated with 95% confidence intervals. Youden index was calculated to obtain diagnostic values for each absorbance measurement. Sensitivity, specificity, positive and negative predictive values were calculated with 95% confidence intervals. Odds ratios were calculated with 95% confidence intervals. Analyses were conducted using R 3.4.3. (www.r-project.org), and easyROC (http://www.biosoft.hacettepe.edu.tr/easyROC) softwares [17,18]. A p<0.05 probability level was considered as statistically significant.
Results
The numbers of participants in each group according to gender (male/female) (ages) were as follows: Group 1 (Good prognosis): 9 (male/female [M/F]: 5/4; 18 ears); Group 2 (Worse prognosis): 15 (M/F: 6/9; 29 ears); Group 3 (Surgical): 7 (M/F: 4/3; 14 ears), and Group 4 (Control): 15 (M/F: 9/6; 30 ears) (Fig. 1). There was no difference in terms of the genders and ages of the patients in the control group and ones with OME (p=0.331 and p=0.690, respectively). The initial immittance measurement revealed Type B tympanogram in 3 (17%) ears in Group 1; 10 (34%) ears in Group 2; and 7 (50%) ears in Group 3. The remaining ears in each study group had Type C tympanogram initially.
The TPP values of all study groups, regardless of the prognosis of the disease, were significantly lower than the control group in the initial measurements (p<0.001). In the following measurements at 1st and 2nd months, the differences between TPP values of the good prognosis group and the control group were insignificant (p>0.05), whereas TPP values of the worse prognosis or the surgical groups were still significantly lower than the control group (p<0.001) (Table 1).

Comparison of the absorbance, resonance frequency and tympanometric peak pressure measures within and between the groups
The analysis of the change of TPP values within the groups by time revealed statistically significant differences in the good prognosis group and the worse prognosis group (p<0.001), which is consistent with the recovery of the disease. The surgical group, in which the ears have undergone VT insertion at the end, stayed stabile in all measurements in terms of TPP values (p>0.05) (Table 1).
RF was another outcome in our study. All of the OME groups, regardless of prognosis of the disease, had lower RF values than the control group at the initial measurement (p<0.001). However, RF values of the ears increased significantly during the follow up in the good and the worse prognosis groups (p<0.001), but not in the surgical group (p>0.05). Statistical analysis revealed insignificant differences between the control group and the good and worse prognosis groups at 1st month and 2nd month measurements, respectively (p>0.05) (Table 1).
In the beginning of the study, the absorbance values of the study groups were lower than the control group at all frequencies, but the differences were significant at 250 Hz, 500 Hz, and 1,000 Hz (p<0.001). Impressively, at 2,000 Hz, initial absorbance values of the ears in the good prognosis group were similar to healthy controls (p>0.05), whereas the other groups were much lower (p<0.001) (Table 1).
During the follow up, absorbance values of the ears in the good prognosis group and the worse prognosis group increased month by month at each frequency. The change was prominent at 500 Hz, 1,000 Hz, and 4,000 Hz for the good prognosis group; absorbance values started from a lower level (p<0.001) but reached the same level with the control group at 1st month measurements (p>0.05). A similar but slower increase arose in the worse prognosis group regarding the absorbance values at 500 Hz, 1,000 Hz, and 2,000 Hz. This finding is consistent with the prognosis of the patients in the worse prognosis group; in which the recovery period of the ears was longer than the ones in the good prognosis group.
One of the remarkable finding was the stability of very low levels of absorbance values in the surgical group at 250 Hz and 500 Hz during the follow up, confirming the findings of clinical examination and conventional tympanometry, which revealed no recovery in those patients (Table 1).
The ROC statistics of the absorbance values revealed significant results for 1,000 Hz and 2,000 Hz for predicting the good prognosis of OME (p<0.05); the absorbance values over 0.237 at 1,000 Hz, and 0.311 at 2,000 Hz have sensitivity and specificity over 70% for predicting the good prognosis of OME (Table 2) (Fig. 2, 3). Furthermore, calculated odds ratios for absorbance measures revealed significant results for 1,000 Hz and 2,000 Hz (p<0.05); and indicated that the ears having an absorbance value over 0.237 at 1,000 Hz, or 0.311 at 2,000 Hz, are 6 times or 5.82 times more likely to recover, respectively (p<0.05) (Table 3).

ROC analyses results and statistical diagnostic measures for absorbances in predicting good prognosis of otitis media with effusion

The receiver operating characteristic (ROC) analysis results for or absorbance measures at the frequencies between 250– 8,000 Hz.

The predictive value of wideband tympanometry. The receiver operating characteristic (ROC) and sensitivity and specificity curves for absorbance measures at 1,000 Hz (A and B); at 2,000 Hz (C and D). Sens., sensitivity; Spec., specificity.
Discussion
The diagnosis and the treatment of OME still have issues that are controversial. Otoscopy is crucial in the diagnosis, better if performed with a pneumatic otoscope. Tympanometry is conventionally performed at 226 Hz frequency and helps verifying the diagnosis. Although tympanometry gives valuable information about the middle ear, in a way is incommensurate. It does not give specific information regarding the middle ear structures and pathologies.
Each of the middle ear structures has different contributions to the total admittance value and tympanometry measures the sum. The evaluation of the middle ear immittance in children with low frequency tympanometry might be inadequate. Studies show that the usage of low frequency tympanometry lacks sensitivity because of stiffness in children and mass effect in adults [19]. High frequency probe tone is more sensitive in systems with stiffness and low frequency probe tone is more with mass effect. While otitis media and ossicular dislocation are examples to mass effected systems; tympanosclerosis and otosclerosis are examples to systems with stiffness.
Whereas conventional tympanometry has limitations regarding the low frequency probe tone, WBT is advantageous because it is capable to measure the minor changes in the mass and stiffness of the middle ear system by using wideband stimulus. We know in general that, the decrease of middle ear pneumatization causes a decrease in absorbance and an increase in the reflectance. However, frequency specific absorbance measures, which are provided by WBT measurement, helps obtaining very detailed information regarding various middle ear pathologies, all of which cause CHL but cannot be distinguished with other audiological tools, such as pure tone audiometry or conventional tympanometry.
In the current study whole parameters of conventional tympanometry were not used, instead, only TPP was used in order to group the patients throughout the study. The reason not using the other parameters than TPP is that the current study does not aim to investigate the value of conventional tympanometry in predicting the prognosis of OME.
There are studies in the literature that compare the conventional tympanometry with WBT. In the study by Keefe et al. [8], the authors measured absorbance and 226 Hz conventional tympanometry in children of age 3 to 8 years with CHL and with normal hearing. They concluded that the WBT absorbance measures predicts CHL more accurate than conventional tympanometry. Piskorski et al. [9] investigated 194 ears of children between 2 to 10 years and found that WBT absorbance measures predict CHL effectively. They`ve also mentioned that 2-4 kHz range is a particularly sensitive indicator of middle-ear status and inclusion of 226 kHz tympanometry may slightly improve the test results. Voss et al. [20], measured reflectance in 8 cadaver ears in cases of positive middle ear pressure, negative middle ear pressure, middle ear effusion, stapes fixation, incudostapedial joint disarticulation and tympanic membrane perforation. They showed that each of these conditions affect the reflectance values. Reflectance was higher under 2,000 Hz frequencies in the ears with stapes fixation and effusion while it was lower in case of tympanic membrane perforation. Interestingly, small perforations showed more differences. However, independent from the size of the perforation, the reflectance of the perforated tympanic membranes was similar to intact ones at the frequencies above 2,500 Hz. In another study performed on 76 ears diagnosed with otitis media and 80 healthy control ears, 4 of the 76 infected ears were found to be normal while 10 of the 80 healthy ears were found to be abnormal on conventional tympanometry [21]. Hunter et al. [6] performed 1 kHz tympanometry, WBT and OAE measurements on 324 newborns, and the participants were divided into two groups as the ones passed the OAE and the ones did not. The authors [6] showed that WBT was more effective indicating middle ear pathologies in patients who did not pass OAE measures. The same study [6] showed that the reflectance in 2 kHz was more sensitive in predicting OAE referral. In the current study, it was also shown that 2 kHz frequency absorbance is significant in predicting OME outcome. It is clear that conventional tympanometry is not capable of distinguishing various middle ear pathologies, but multi-frequency tympanometry seems to be. However, still the conventional tympanometry is the standard method whose normative values are clearly defined for each type of pathologies for different age groups. WBT still lacks the normative data for many middle ear pathologies and cannot be considered as a primary choice of impedance audiometry in the daily clinical practice. Therefore it is a hot topic in scientific research and we wanted to evaluate the value of WBT for prediction of OME which has not been previously studied.
There are several studies in the literature investigating the absorbance and reflectance changes due to effusion in the middle ear. Ellison et al. [22] performed WBT prior to surgery in patients who were planned to have VT insertion for OME and compared the results with healthy volunteers. They showed that the absorbance decreases in the ears with effusion especially at 1.5-3 kHz interval. Beers et al. [23] compared the children having OME with healthy ones and found that the reflectance was higher in the effusion group between 680 Hz and 6,000 Hz. They’ve mentioned that frequencies over 800 Hz are more reliable showing OME. The same study suggested that the reflectance measure at 1,250 Hz is superior to 226 Hz static admittance measure in detecting the middle ear effusion. Voss et al. [20] showed that in the middle ear effusion model, the reflectance was minimal when less than 50% of the middle ear was filled with fluid but it increased as well in most frequencies when the fluid volume increased. Piskorski et al. [9] and Feeney et al. [24] showed in their studies that, up to 2,000 Hz frequencies the reflectance value is close to 1 in cases with middle ear effusion. However, we demonstrated in the current study that the absorbance levels are lower in the ears with OME than healthy ones not only at a specific frequency region, but from 250 Hz to 8,000 Hz at all frequencies that we have measured, low frequencies were affected more, though. Furthermore, our data indicates that higher the absorbance at 1 and 2 kHz frequencies, better the prognosis, which is a remarkable and novel finding. Also, in synchrony with the recovery of OME, absorbance measures increase significantly at 250 Hz, 500 Hz, 1,000 Hz, and 4,000 Hz. On top of this, analysis of ROC statistics and calculation of Youden index for the absorbance measures revealed significant results for 1,000 Hz and 2,000 Hz; diagnostic values were detected as 0.237 and 0.311 for the absorbance measures at those frequencies, respectively. Usage of these diagnostic values, have sensitivity and specificity over 70%, and up to 88% of negative predictive value in prediction of the good prognosis of OME patients. It is very well known that OME can cause 25 to 30 dB of hearing loss which may potentially delay speech and language development in a child [13,14,25]. Being able to predict the poor prognosis will absolutely accelerate the decision of surgical treatment which will shorten the period with CHL. We suggest WBT as a potential objective measurement tool for prediction of the prognosis of OME nevertheless it can be used if supported with further validation studies with larger populations.
RF is a value that can be measured by WBT. The studies show that the RF value in the normal ears is between 650-1,400 Hz with a mean of 950 Hz. Consistently with the literature, the mean RF of healthy ears in our study was 1,104 Hz. There are studies showing that the RF value increases in case of otosclerosis, ossicular fixation, and rheumatoid arthritis [26,27]. On the other side, some pathologies, such as OME, tympanic membrane atelectasis, otitis externa, ossicular dislocation, and large vestibular aqueduct can cause a decrease of RF [21,28]. Our data suggested the same; compared with the healthy controls the ears with OME had significantly lower RF values. Moreover, RF values increased with the recovery of OME. According to those findings it can be quoted that RF is a reliable indicator of the status of the middle ear and can be used as a measure to confirm the findings of otoscopic examination and conventional tympanometry for an accurate diagnosis.
The current study has also some limitations. The sample size is relatively small which limits its possibility to generalize the results through the whole population. The hearing values could not be analyzed because of the age differences of children and further studies using the hearing levels as a parameter would strengthen the results.
As a conclusion, we have investigated the capability of WBT for the prediction of the prognosis of OME. Standing on our data, we assert that higher absorbance values at 1,000 and 2,000 Hz indicates better prognosis of OME. Our analysis suggested diagnostic values for absorbance measures at 1,000 Hz and 2,000 Hz, which has never been done before. However, extended studies including higher number of participants are needed in order to confirm our findings. Further research may put WBT into routine use for the assessment of OME patients in the near future.
Acknowledgements
None
Notes
Conflicts of interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Mehmet Ilhan Şahin, Duygu Demirkan Özyürek, Ibrahim Ketenci. Data curation: Duygu Demirkan Özyürek, Alperen Vural. Formal analysis: Mehmet Ilhan Şahin, Gökmen Zararsız. Methodology: Mehmet Ilhan Şahin, Ibrahim Ketenci. Project administration: Mehmet Ilhan Şahin, Duygu Demirkan Özyürek, Alperen Vural. Visualization: Mehmet Ilhan Şahin, Ibrahim Ketenci, Yaşar Ünlü. Writing—original draft: Mehmet Ilhan Şahin , Duygu Demirkan Özyürek, Alperen Vural. Writing—review & editing: Mehmet Ilhan Şahin, Alperen Vural, Ibrahim Ketenci, Yaşar Ünlü. Approval of final manuscript: all authors.

