Health-Related Quality of Life in Children With Cochlear Implants From Parents’ Perspective
Article information
Abstract
Background and Objectives
To evaluate the health-related quality of life (HRQoL) in parents of children with cochlear implants and assess influencing factors. These data can enable practitioners to support patients and their families in utilizing the cochlear implant and its benefits to the fullest extent.
Subjects and Methods
A retrospective descriptive and analytic study was conducted at the Implantation center Mohammed VI. Parents of cochlear implant patients were asked to fill out forms and answer a questionnaire. Participants included parents of children <15 years old who underwent unilateral cochlear implantation between January 2009 and December 2019, presenting with bilateral severe to profound neurosensory deafness. Participants completed the children with cochlear implantation: parent’s perspective (CCIPP) HRQoL questionnaire.
Results
The mean age of the children was 6.49±2.55 years. The mean time between implantation for each patient and this study was calculated as 4.33±2.05 years. There was a positive correlation between this variable and the following subscales: communication, well-being and happiness, and the process of implantation. For these subscales, the score was higher as the delay was greater. Parents of children who received speech therapy before implantation were more satisfied on the following subscales: communication, general functioning, well-being and happiness, implantation process, implantation effectiveness, and support for the child.
Conclusions
The HRQoL is better in families of children who received their implant at an early age. This finding raises awareness of the importance of systemic screening in newborns.
Introduction
According to a Center for Disease Control and Prevention report published in 2019, Congenital hearing loss represents 1.7 per 1,000 newborn [1] in the US, and the prevalence of hearing loss among children between 6-19 years of age was 14.9% of children based on the work of Niskar, et al. [2] As it is well known, hearing loss in children leads to other disabilities in 40%-50% of cases [3].
The cochlear implantation (CI) for congenital deafness in children has revolutionized the otological field in so many ways, permitting the acquisition of the hearing sense, the development of communication skills, and integration of social life, with a lesser risk of developing additional conditions [3,4].
Multiple health-related quality of life (HRQoL) questionnaires have been developed over the years and some of them were specific to the CI. These questionnaires were both addressed to the pediatric population after the surgery and to their parents [4].
O’Neill, et al. [7] developed the “The children with cochlear implantation: parent’s perspective (CCIPP),” a closed set specific CI survey based on the parent’s point of view. It is divided into 10 subscales. The CCIPP is the most used questionnaire by implantation teams [8].
The aim of our study is to evaluate the HRQoL in parents of children with CI and to assess the factors that might influence it, so we, as practitioners, would act on them to allow the patients and their families to take full advantage of the CI and its benefits in their daily lives.
Subjects and Methods
A total of 70 chilren were included. The parents gave verbal consent to participate in this study. This study was conducted in accordance with the Declaration of Helsinki.
We conducted a retrospective descriptive and analytic study. This study included all children <15 years old when implanted, presenting a bilateral severe to profound neurosensory deafness who underwent unilateral CI between January 2009 and December 2019 in our implantation center, at least 2 years after their implantation surgery. The exclusion criteria as follows:
• >15 years old,
• With neurosensory deafness associated with abnormalities,
• Cerebral palsy,
• Patients who underwent bilateral implantations, and reimplantations.
• Plus the Absolute contraindications:
- Major inner ear malformations,
- Complete cochlear ossification,
- Cochlear nerve agenesis,
- And in case of major anesthetic risk (implantation under local anesthesia is impossible in children).
Patients data was collected from medical files in the same center; data like patient’s history, epidemiology and patient characteristics. The HRQoL questionnaire used was the Nottingham Pediatric Cochlear Implant Program “CCIPP” (Nottingham University Hospital, Nottingham, United Kingdom). The questionnaire was composed of 10 subscales: communication, general functioning, self-reliance, well-being and happiness, social relationship, decision to the implant, education, the process of implantation, supporting the child, and effect of implantation. The parents’ answers to the questionnaire were rated as strongly agree, agree, neither agree nor disagree, disagree, and strongly disagree.
The parents completed the form in a special consult after agreeing to participate in the study, using the help of the doctors in charge of the study.
We used IBM SPSS 25.0 (IBM Corp., Armonk, NY, USA), to perform the statistical analysis. Frequencies, mean, median, standard deviation, and percentages were used to assess the data distribution.
The Spearman nonparametrical test was used to search for the correlations between descriptive data of the study and the relationship with the change of the subscales scores. A value of p<0.05 was considered statistically significant.
Results
We collected the data from 70 patients; the mean age was 6.49±2.55 years ranging from 1 to 12 years old. The most found age interval was between 5 and 7 years old children. There were more female than male patients representing 57.1% of cases. Our patients’ families were mostly of low social and economical levels living in urban areas, according to our country’s classifications. Parents had a secondary academic level in most cases and 10% of them were unschooled and 21.4% made it to primary school. Few mothers were working and representing 7.1% of all cases. Two sub-groups represented the medical coverage: patients with health insurance (31.4%) and patients with social security (a national program for destitute families) representing 65.7%, finally there were 2.9% of patients with no medical coverage (Table 1).
The patient’s history found was mostly a history of meningitis in 8 cases, neonatal jaundice in 2 cases, and history of cranial trauma in 2 cases.
The child’s deafness was discovered in most cases when patients presented language acquisition disorder and the age of the first consult was before 2 years old. All our patients benefited from a tonal and/or behavioral audiometry, an otoacoustic emission and acoustic evoked potential under general anesthesia, a CT scan and an MRI before the decision to implant. They also benefited from a psychological speech therapy consult that helped us know their psychological condition and their communication mode.
The indication to implant was decided upon the age and the audiometric findings. The distribution of patients according to their demographic characteristics and the status of the child is shown in Table 1, with the number and percentages of patients in each category.
The time between the implantation and this study was calculated in years in each patient with a mean of 4.33±2.05 years ranging of from 2 to 9 years. There was a positive correlation between this variable and some scores of subscales: communication (p=0.002), well-being and happiness (p<0.001), and the process of implantation (p=0.001), the score was higher as the delay was greater (Fig. 1). Fig. 2 is a box-plot chart with mean scores in all quality of life domains. The statistical study objectified a correlation between age and well-being and happiness (p=0.005), the process of implantation (p=0.029) subscales. The younger the patients, the more satisfied were the parents. Gender was not correlated to any subscale score. The mother’s profession was correlated to the process of implantation (p=0.003) and the supporting the child (p=0.028) subscales, stay at home mothers were more satisfied in terms of this study.

Box-plots for the time (from implantation to the study) and subscale scores. A: Communication scores (p=0.002). B: Well-being and happiness scores (p<0.001). C: The process of implantation scores (p=0.001)
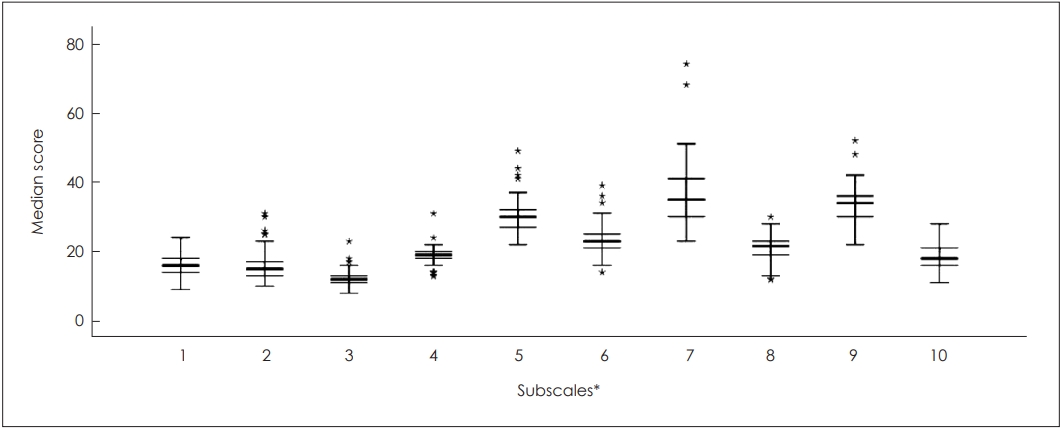
Box-plot chart with mean scores in all quality of life domains. *Subscales: 1, communication; 2, general functioning; 3, self-reliance; 4, well-being and happiness; 5, social relationships; 6, education; 7, process of implantation; 8, effects of implantation; 9, decision to implant; 10, supporting the child.
Parents of children who received before implantation a speech therapy were more satisfied in terms of communication (p=0.043), general functioning (p=0.012), well-being and happiness (p=0.048), the process of implantation (p=0.002), effect of implantation (p=0.017) and supporting the child (p=0.008) subscales. They were highly more satisfied than the parents of children who did not benefit from a speech therapy before the implantation (Fig. 3). This was also the case for parents of children who were implanted early compared to those who had late implantation in the well-being and happiness (p=0.037) and education (p=0.004) subscales (Table 2 and Fig. 4).
Table 2 regroups the nonparametric correlation results between the different variables and the subscales of the questionnaire. The rest of the plot’s representation of correlated variables to different subscale scores is presented in Fig. 5. The CCIPP subscales were intercorrelated for most of them, except for the effect of implantation subscale which was not correlated with any other questionnaire subscale. Supporting the child was not correlated to the well-being and happiness subscale (p=0.095) (Table 3). Table 3 regroups the correlations between the different subscales of the questionnaire.

Box-plots for the age of appearance and the self-reliance score (A), the history of using hearing aids and the self-reliance score (B), communication mode and the self-reliance score (C), psychological assessment and well-being and happiness score (D), schooling status and the effect of implantation score (E).
Discussion
In a study about the history of CI, Ramsden stated that after concentrating on conductive hearing loss in past decades, otology is entering a new era of sensory hearing loss [3]. CI has known a big evolution in the last century, it started in the 17th century with Duchenne of Boulogne when he first stimulated an ear with electricity. Then many years later Dr. House managed to invent the very first single electrode cochlear implant, afterwards with the development of technology and science the multi-electrode implant we have nowadays have seen the light of life [4].
The main purpose of CI is to provide sound awareness in deaf patients by stimulating different areas of the cochlea [5]. It provides speech comprehension and high intelligibility, even conversations over the phone [4].
All these researches allowed to revolutionize the otology world, making members of families with neurosensory deafness acquire the hearing sense and thus the ability to speak and have a normal social integration.
The burden and stress of having a disabled child and the mental pressure resulting from it, is a real problem for parents, considering the social, intellectual, and behavioral abnormalities arising from lacking an essential sense for a so-called normal life [6]. Multiple studies have treated this subject and the conclusion is that parents with impaired children were more luckily to develop mental health issues [6-8].
Vieira, et al. [9] conducted a study about the family’s perspective on the cochlear implant and concluded that for the parents the cochlear implant alone meant a better future for their children, not considering that the main actor in the processes of the child’s rehabilitation and the success of this whole process is the family itself. Which makes these kinds of studies important; understanding the family’s difficulties and the factors that might influence the quality of life in this families [10,11].
Studies were conducted over the years to assess the HRQoL in children with a cochlear implant using different questionnaires; most of them used the parent’s perspective instead of considering the children’s point of view [12].
We used the CCIPP, the same questionnaire was used by multiple studies published [8,9,12-17].
The correlation between the questionnaire subscales was evaluated, and it was found that the communication subscale was positively correlated with most subscales in our study, the same results were obtained by other researchers [8,12-14,17], and according to Kumar, et al. [17], this is explained by the fact that from the parent’s point of view a better communication skills implicates better self-reliance, a better education, better social interaction, and mostly achieving greater happiness. On the other hand, Alkhatani, et al. [15] findings were different. This could be due to the small sample they studied, as only the social relationship subscale was correlated to the well-being and happiness subscale.
The other important parameter that was studied, was the time of use of the cochlear implant before the parent’s submission of the CCIPP questionnaire, in all different papers published the longer the time frame the higher the parent’s satisfaction [9,13-17,18,19], and our results match those found in the literature review. We also found out that the longer the children had their implant the highly satisfied were the parents with the process of implantation and the decision to implant subscales.
In a systematic review conducted in 2021, only studied in few papers studied their correlation with the questionnaire results [12], two out of these studies, Alkhatani, et al. [15] and Vieira, et al. [9], used the CCIPP questionnaire and it was found that the age of implantation was associated with a greater quality of life score, our findings corroborate the ones in the literature. Consequently discovering the congenital deafness by systematic screening and by raising awareness about congenital deafness, would allow us to implant children at a younger age and hence get better results.
Contrastingly as was stated by Vermi Sli Peker, et al. [20], demographic characteristics and patients’ history should be taken into account as they might influence the parent’s perspective and would help us point out the variables to act on.
In this study, we also found that parents of children who received hearing aid and speech therapy before the CI were more satisfied than others. We did not find any previous studies discussing this parameter.
The limitation of this study is mostly the questionnaire used to assess the HRQoL from the parent’s perspective, as the questionnaire has no consensual calculation process nor an interpretation scale [14,16].
Overall, parents were satisfied with the CI results in their children [17,19,21-28], but more studies should be done on this subject to have a better knowledge of the factor that might influence the HRQoL, and act on the findings to enhance the effect of the CI.
In conclusion, parents’ expectations from the CI are not only for their children to acquire hearing sense, but also to have better communication skills, education level, and integrate the social life. In our study, the HRQoL is found to be better in families in which children were implanted at an early age, the younger the children (<5) the greater were the score satisfaction (p<0.001); this finding raises awareness of the importance of systemic screening in newborns. Psychological support should also be encouraged for both children and parents to allow better social integration.
Acknowledgements
None
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Sara Rochd, Othmane Benhoummad. Data curation: Salma Salhi, Mohammed Amine Ait Lhadj. Formal analysis: Sara Rochd. Methodology: Sara Rochd, Youssef Lakhdar. Supervision: Othmane Benhoummad, Abdelaziz Raji. Visualization: Youssef Rochdi. Writing—original draft: Sara Rochd. Writing—review & editing: Othmane Benhoummad, Abdelaziz Raji. Approval of final manuscript: all authors.





