Introduction
Deception is an act or statement, which misleads, hides the truth, or promotes a belief, concept, or idea that is not true, usually for personal gain or advantage [
1]. Intent is critical with regard to deception, as it differentiates itself from an honest mistake.
Deception does not occur frequently in audiology, however, non-organic hearing disorders (NOHD) should be considered in everyday audiological practice. Such disorders may involve otherwise normal individuals, who are seeking personal or economic gains, or people, who exaggerate a mild hearing loss, or pretend to be profoundly deaf in the context of a legal dispute, or even individuals, who have emotional or psychological disorders, and are in seek of attention or constant hospitalization. Cases of alleged hearing adequacy, when this represents a prerequisite for professional evolvement, complete the spectrum of NOHD.
The assessment of suspected NOHD patients should be prompt, and the methodology employed should comprise testing, which would be quick, adequate, objective, and easily repeated. Auditory steady-state response (ASSR) represents such an objective method of hearing asssessment, which can reliably distinguish NOHD from actual hearing loss in doubtful cases.
The aim of the present case series was to describe all the possible facets of NOHD and emphasize the superiority of ASSR, compared to previously employed hearing assessment tools.
Subjects and Methods
A series of seven patients with NOHD were assessed at the Audiology Unit of Attikon University Hospital. Three of them were males, and four females. The age of the examinees ranged between 17 and 59 years.
The audiological evaluation comprised tympanometry, pure-tone audiometry, and ASSR testing, and the results were complemented by auditory brainstem responses (ABR), and otoacoustic emissions (OAEs). The research protocol was submitted, and received ethical approval by the Ethics Committee of the University of Athens (IRB approval no: 1415014762–08/05/2015), prior to commencing data collection. All procedures were in accordance with the 2013 Helsinki declaration. Participants were asked to sign a consent form before being enrolled in the study.
With the patient in a relaxed position in a soundproof chamber, 40 Hz stimulus rate CE-chirp® sounds are given through insert phones (adult awake protocol). The device used is the Eclipse EΡ 25TM (Interacoustics, Middelfart, Denmark). The examination time is 6 minutes per examined hearing level (HL). A given stimulus of 20-30 dB higher than the least threshold in four frequencies of the pure tone audiogram (500, 1,000, 2,000, and 4,000 Hz) is presented in both ears at the same time. Whenever, the curve of the stimulus reaches 100% certainty, it turns green (positive outcome), and the operator lowers the stimulus by 10 dB. If the curve remains under 100% by the end of the examination time, the outcome is negative. The examiner may choose to extend the testing by 1 minute, if he/she believes that a positive outcome is likely to occur. An estimated audiometric curve is obtained, based on the least threshold stimuli of the four examined frequencies, producing a positive outcome, at the end of the test. The perceived threshold is automatically transformed from dB sound-pressure level to dB HL, thus obtaining a reliable estimate of the pure-tone audiogram.
Case descriptions
Munchausen syndrome
Munchausen syndrome is a psychological disorder, where a person pretends to be ill, or deliberately produces symptoms of illness in him/herself. The main intent is to assume a “sickness role,” which would place the person at the centre of care and attention, without, however, any other practical benefit from this pretense (i.e., claiming an incapacity benefit). Possible causes of Munchausen syndrome include childhood trauma, personality disorders, or antipathy against authority figures or healthcare professionals.
All three patients in the present series were females between the second and third decade of their lives. Two of them presented with acute bilateral deafness, whilst the third initially presented with unilateral, followed by bilateral hearing loss in the following three months. Past medical history revealed irritable bowel syndrome in the two older patients, whilst the socio-environmental living conditions in two of the patients were challenging.
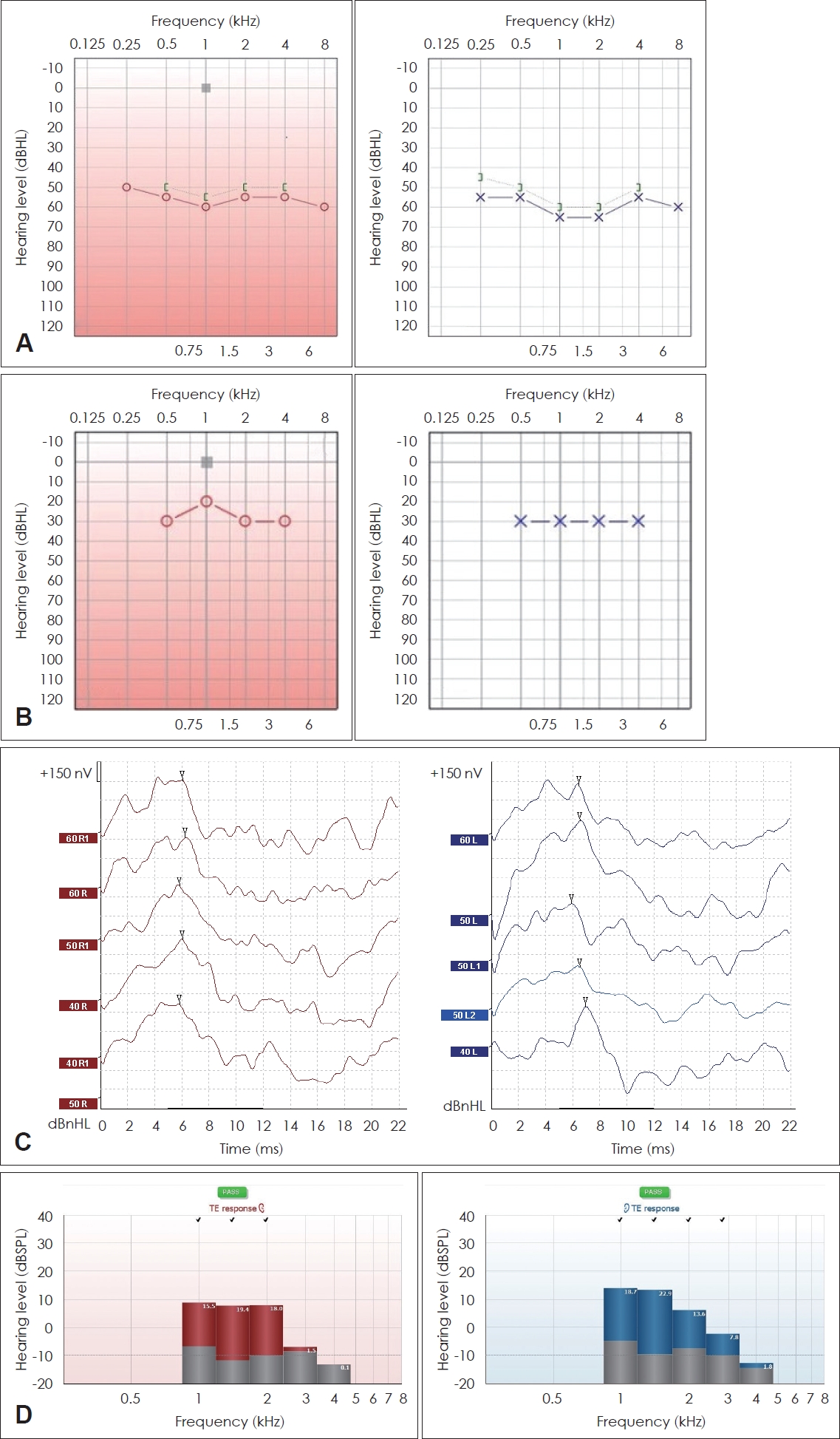
Clinical ENT examination was unremarkable in all cases, and the tympanometric curves were suggestive of normal middle ear ventilation. Audiometric testing was suggestive of severe to profound hearing loss, bilaterally in two cases, and initially unilaterally, followed by contralateral hearing impairment within three months, in the third case (
Fig. 1A). However, the non-significant impairment in the communicative abilities of all patients, largely inconsistent with the audiometric curves, along with previous hospital admissions for various reasons, necessitated ASSR assessment, which proved normal in all patients (
Fig. 1B). ABR and OAEs were also indicative of normal hearing (albeit not being frequency-specific) (
Fig. 1C and
D, respectively). Treatment for sudden sensorineural hearing loss was discontinued in all patients, who were subsequently referred for psychiatric evaluation.
Malingering
Three patients in the present series intentionally feigned profound hearing loss. These comprised two males and one female patient. The socio-economic background among the three individuals differed. One was a male economic refugee, who sought state benefit, by claiming profound bilateral hearing loss. A second male patient was an ex-soldier claiming compensation by the Greek Military for unilateral deafness, as a result of a grenade explosion. The third patient was a female, who had been receiving state benefit for incapacitation, due to profound bilateral hearing loss, for the past 40 years, and was re-examined, following strong reservations about her hearing loss from the State Otorhinolaryngologist.
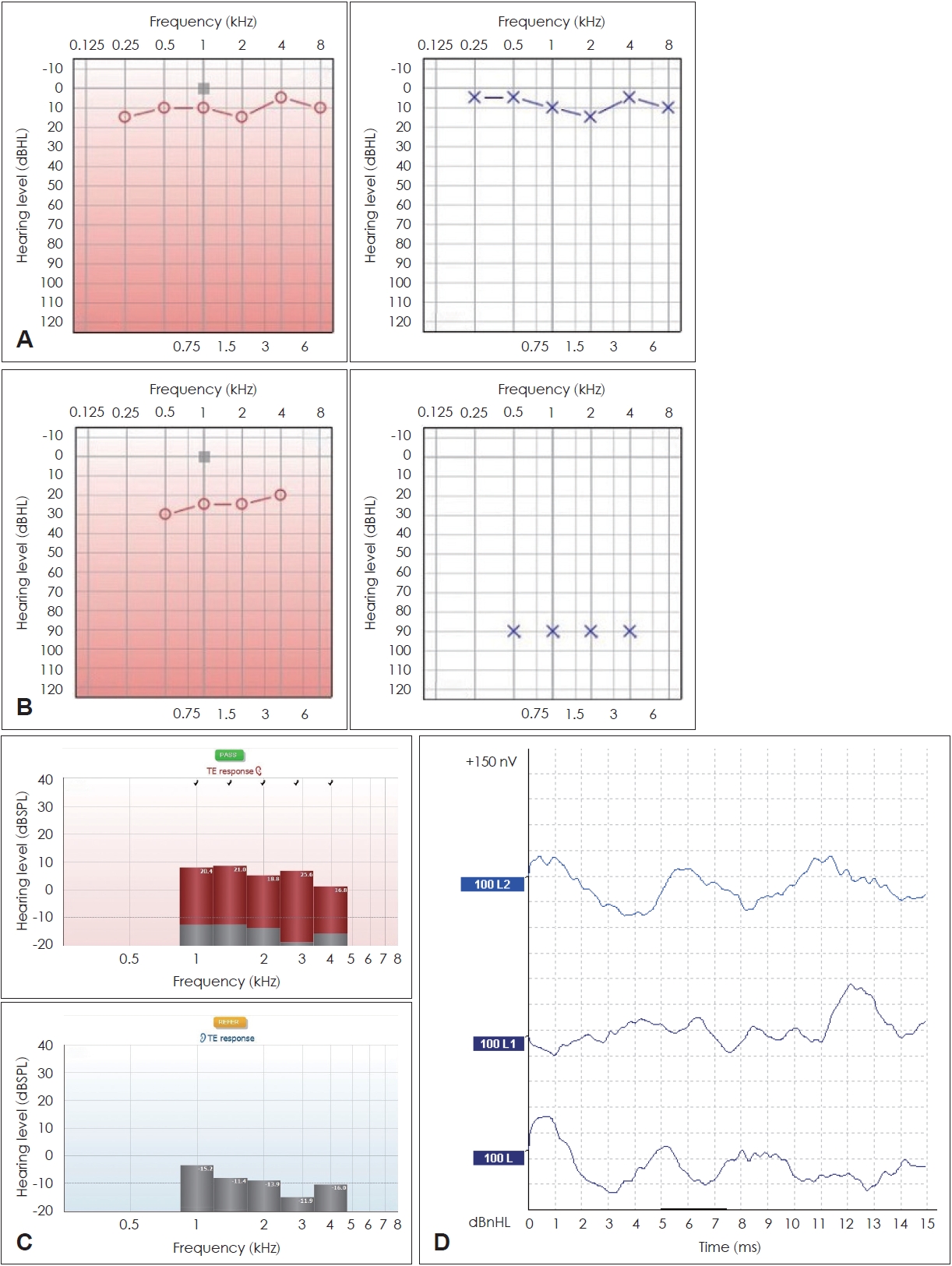
Clinical ENT examination was unremarkable in all cases, and the tympanometric curves were suggestive of normal middle ear ventilation. Audiometric testing was suggestive of profound hearing loss, bilaterally in two cases, and unilaterally involving the right ear in the third case (
Fig. 2A). Interestingly, the communicative abilities of all patients appeared significantly impaired. ASSR assessment proved normal with regard to the male patients (
Fig. 2B), and demonstrated mild hearing loss in the low and severe in the high frequencies in the female patient (not justifying any state benefit). ABR and OAEs were also indicative of normal hearing in the male patients. The female patient did not elicit OAEs (
Fig. 2C), and the respective ABR curves were suggestive of mild hearing loss (
Fig. 2D).
Other NOHD facets
A 50 year-old career naval officer was due to be promoted, having as a prerequisite, however, normal hearing thresholds. Clinical ENT examination was unremarkable, and the tympanometric curves were suggestive of normal middle ear ventilation. Audiometric testing was considered unreliable, due to potentially random responses to the pure tones administered (
Fig. 3A). ASSR assessment proved normal in the right ear, but revealed profound hearing loss in the left ear (
Fig. 3B). OAEs were also not elicited in the left ear, albeit being present in the right ear (
Fig. 3C), whilst the respective ABR curves were suggestive of profound hearing loss in the left ear (
Fig. 3D).
Discussion
NOHD is a multi-faceted condition encompassing various etiologies. Munchausen syndrome, malingering, or even avoidance behavior should be suspected in cases of flat pure tone audiograms, quite often inconsistent through series of examinations, provided by people with normal voice control, satisfactory communicative abilities, and obvious interests for obtaining some sort of benefit [
2,
3].
The accurate determination of NOHD has been intensively pursued by healthcare providers in the past. The methodology employed mainly involved subjective hearing tests (i.e. Stenger test, Carhart test, Lombard voice intensity test, or lateralization test) [
4], whilst ABR represented an objective examination method, which previously served as the gold standard [
5]. However, not only are ASSR thresholds closer to the actual audiometric thresholds, compared to ABR testing, in the presence of hearing impairment [
6], they are also superior, when the corresponding pure-tone audiogram is widely ranging between adjacent frequencies [
7], or when the obtained ABR curves are not easily distinguished.
Furthermore, subjective hearing tests are often more useful in unilateral pseudo-hypacousis (i.e. Stenger test, lateralization test) [
8], whilst a determined person of average ability may learn to modify his/her voice in the presence of unilateral noise, thus invalidating such tests [
9]. In addition, a degree of underlying organic hearing loss could perplex the determination of the functional (non-organic) component in NOHD cases. Indeed, it is not surprising that in a large study involving 200 military candidates, the positive predictive value of the Stenger test in verifying unilateral profound hearing loss, did not exceed 87.5% [
10].
The value of ASSR testing stems from the fact that it can reliably indicate the actual HLs levels in four main frequencies (500, 1,000, 2,000, and 4,000 Hz) by obtaining a valid estimated audiogram through the use of statistical measures [
11]. This is materialized, due to the physical properties of CE-chirp
® sounds, which are used as auditory stimuli, which bypass the natural course of cochlear response to sound, in which the basal turn is reacting first. The CE-chirp
® sounds stimulate the lower frequencies in the apical turn of the cochlea first, and through time delay subsequently the mid and basal turn of the cochlea. This results, in turn, to simultaneous cochlear firing and massive brainstem response, which is picked-up by the active electrodes, and, when mathematical prerequisites are fulfilled, is transformed to estimated HLs. More than one response from each ear can be recorded at the same time with a maximum of eight (four in each ear). Nevertheless, since most NOHD cases report profound levels of hearing impairment, it is considered safer to present one stimulus in each ear separately in order to ascertain the reliability of the obtained results.
On the other hand, ABR testing could be a useful adjunct in cases of NOHD, as it could confirm the results of the ASSR testing by adding two further advantages. The stimulus is a broad-spectrum click ranging between 2,000 Hz and 4,000 Hz, hence bearing different physical properties, than the corresponding ASSR stimulus. Obtaining comparable results with different auditory stimuli confirms the soundness of NOHD diagnosis. Furthermore, the examiner is more actively participating in the diagnostic process by personally recognizing the waveform, which corresponds to the patient’s HL instead of relying on a device, to perform all the necessary mathematic calculations.
Finally, the diagnosis of NOHD is completed by recording the OAEs, which represent the response of a normally functioning inner ear to an externally administered click stimulus [
12]. In contrast to ASSR and ABR testing, both of which assess the acoustic output of sound (i.e. what reaches the central nervous system), OAEs assess the acoustic input of sound (i.e. what reaches the target-organ), and their presence is indicative of normal (or near-normal) cochlear function.
A non-confrontational approach should be adopted by ENT physicians, towards cases of suspected NOHD. That is because confrontation rarely leads to admission of the behavior or resolution of the problem, and this applies both for patients with a psychiatric background, and for those who are feigning hearing loss. Indeed, it is not uncommon, for many patients belonging to the latter category, to be experiencing at least some degree of underlying organic hearing loss [
13]. However, the certainty that ASSR testing provides, along with the confirmation from the ABR and OAE arms of the testing battery, which should be routinely performed as complementary testing for NOHD diagnosis, when a discrepancy between pure tone audiometry and ASSR results is noted and in line with the audiological principle of result cross-checking, warrants immediate discontinuation of any ENT medication and psychiatric referral in the former patients, and notification of the appropriate authorities in the latter cases. Psychiatric counselling may also be required in cases of alleged hearing adequacy when this represents a prerequisite for professional evolvement.
In conclusion, NOHD is a multi-faceted condition encompassing various etiologies. ASSR testing represents an objective and reliable method of hearing asssessment, which can serve as a gold standard in distinguishing NOHD from actual hearing loss. The use of ASSR is, therefore, strongly recommended in suspected NOHD cases, bearing medical or medico-legal implications.