|
 |
- Search
| J Audiol Otol > Volume 26(4); 2022 > Article |
|
Abstract
Background and Objectives
We present the anatomical and functional results on the use of cartilage in myringoplasty and use the data to analyze the factors influencing hearing gain.
Subjects and Methods
This retrospective study included 161 cases of cartilage myringoplasties collected over an 11-year period (2010-2020). Of the 161 cases, the etiology of the tympanic perforations was simple chronic otitis media in 154 (95.65%) ears and traumatic in 7 (4.35%) ears. The mean preoperative Rinne was 26.20±7.05 dB. The most commonly used approach was retroauricular, and the common graft material was tragal or conqual cartilage.
Results
After the follow-up period (mean:15 months), the anatomical success rate was 93.2%; there were nine cases of reperforation, of which three were reoperated with a good final result. The hearing success rate (residual Rinne ≤20 dB) was 91.9% with an average gain of 11.48±8.62 dB. The only factor significantly influencing the anatomical outcome was the history of chronic rhinosinusitis. In univariate studies, several factors influencing the functional result were revealed; the only one retained after elimination of bias was the anatomical result.
Myringoplasty or tympanoplasty type 1 is a surgery aimed at repairing a tympanic perforation. Tympanic perforations are most often resulting from chronic otitis media (sequelae of chronic otitis media) [1]. Recently the use of cartilage has become very popular among otologists who recommend it as the graft of choice due to its better results than other materials for tympanic membrane repair [2]. In our country, cartilage was introduced in the late 1990s and has been widely used by several surgeons ever since. Initially, the stiffness of the cartilage raised some concerns about its impact on the hearing result, but several studies have dissipated these doubts given the satisfactory functional results they have obtained [1,2].
Cartilage myringoplasty has yielded very satisfactory in different series [1,3-5]. The purpose of this study is to present the anatomical and functional results of a series of 161 cartilage myringoplasty procedures and to justify the selection of cartilage as the material of choice in the repair of tympanic perforations, while specifying the predictive factors of failure in this surgery.
We carried out a retrospective study involving 150 patients who underwent myringoplasty over an 11-year period extending from January 2010 to December 2020. Eleven patients had surgery on both ears and a total number of 161 myringoplasties were performed during the study period. We included patients who presented with a simple tympanic perforation and who underwent a cartilage myringoplasty with a minimum postoperative follow-up of 3 months. All patients operated on for retraction pockets or chronic cholesteatomatous otitis media were excluded from this study. Pre- and postoperative baseline tonal audiometry, performed systematically in all patients, was used to evaluate the average auditory threshold in air conduction and in bone conduction at the following frequencies: 500, 1,000 and 2,000 Hz. A CT scan of the temporal bone was indicated in patients with a considerable audiometric Rinne (>45 dB), and therefore, a suspected lysis of the ossicular chain. In addition, a follow-up CT scan after myringoplasty was indicated in patients with functional failure. The majority of patients were operated via the retro-auricular approach (Fig. 1). The harvested cartilage is either conqual or tragal. The graft is placed either under or over the malleus handle, or a notch is made in the cartilage to fit the malleus handle (Fig. 2). Making a notch in the cartilage graft that will hug the handle of the malleus has two advantages: graft stability (inhibit sliding movements of the graft) and lower risk of iatrogenic cholesteatoma (do not cover the epidermal residue on the handle of the malleus).
Postoperatively, patients were monitored clinically, audiometrically and in some cases by radiology (CT-scan). Anatomical results were interested in the condition and position of the graft: healthy, inflamed, reperforated or displaced. We recorded the postoperative hearing thresholds, specifying the audiometric gain. The important parameter calculated was the residual Rinne which was obtained by the average difference between the postoperative air conduction hearing threshold and the preoperative bone conduction threshold. A good functional result was defined by a residual Rinne of 20 dB or lower.
Statistical analysis was performed using SPSS version 21 software (IBM Corp., Armonk, NY, USA). The Student’s t-test was used to compare the means for quantitative variables of independent series, and the Pearson’s chi-square test (χ2) was used to compare percentages. Using uni- and multivariate studies, we determined the factors influencing anatomical and functional outcomes after surgery. The significance level was set at p<0.05.
This study was approved by the ethics committee of our institution. We have obtained the informed consent of the patients to carry out this study based on the collection of hearing thresholds before and after surgery, while respecting anonymity and ensuring that the manuscript does not reveal any identity of our patients.
The study population consisted of 150 patients with a mean age of 33 years (range 9 to 68 years). The pediatric population aged under 16 years old represented 14% (21 children) of all cases. Among the children, three (13%) were operated for adenoidectomy and two (8.7%) had tympanostomy tubes. Of the 161 cases, the etiology of the tympanic perforations was simple chronic otitis media in 154 (95.65%) ears and traumatic in 7 (4.35%) ears. In 24 patients, there was a history of otologic surgery (myringoplasty by the temporal muscle aponeurosis or cartilage) in therapeutic failure (reperforation). Our patients presented mainly with chronic otorrhea (90%) and hypoacusis (87%). Tinnitus was reported in 23% of cases and vertigo in 5.7%. In our study, the interval between the last otorrheic episode and the date of myringoplasty ranged from 1 month to 2 years, with an average of 5 months.
Tympanic perforations were anterior in 19.9% of cases, posterior in 15.5%, inferior in 8.1%, and central in 56.5%. The size of the perforation was greater than 50% of the tympanic surface in 96 cases (59.6%). Examination of the contralateral ear showed a complete and normal eardrum in 54% of cases, a tympanic perforation in 30.4%, a retraction pocket in 1.9%, a myringosclerosis in 6.9%, and complete graft in 6.8% (11 patients in our series were operated on both sides). On tone audiometry, conductive hearing loss was noted in 138 cases and mixed hearing loss in 23 cases. The average air conduction hearing threshold was 36.1 dB with an average Rinne of 26.2±7.05 dB.
The approach was retroauricular in 157 ears (97.5%). The transcanal approach, indicated for small inferior perforations with a good caliber external duct, was used in 4 ears (2.5%). The mucosa of the tympanic cavity was healthy in 133 ears (82.6%) and inflammatory in 28 ears (17.4%). The ossicular chain was complete and mobile in 143 ears (88.8%). The handle of the hammer was medialized (horizontalized) in 18 ears (11.2%), which were released by the section of the spatula adhering to the internal wall of the tympanic cavity. The revitalization of the edges of perforations was not done systematically but reserved for the edges which tend to roll up and to invaginate into the interior of the tympanic cavity (19%). The anterior wall is peeled off in case of anterior perforations or large perforations including the anterior quadrant.
The underlay technique was used for positioning the graft in all cases (100%). The material used was tragal cartilage in 42.2% of cases and conqual cartilage in 58.8% of cases placed. The cartilage graft was reinforced with temporal muscle fascia in 55.9% of cases (we do not place any support below the cartilage graft). We do not put the cartilage graft in palisade, but in toto-cartilage, and if there is a free gap between the eardrum and the graft, it is filled with perichondrium. At the end of the intervention, we put on a self-absorbable dressing (Surgicel®; Ethicon Sàrl, Neuchatel, Switzerland).
The average length of postoperative hospital stay was 3 days. An infection of the surgical wound was noted in 6 ears (3.72%) requiring appropriate antibiotic therapy with daily local care. The average duration of follow-up was 15 months (between 6 and 96 months). During this follow-up, a good anatomical result (defined as complete and definitive closure of the perforation, good condition of the graft, and a good caliber external auditory canal) (Fig. 3) was found in 150 ears, accounting for 93.2% of the cases. Anatomical failures were represented by reperforation of the graft in nine ears (5.6%) and chronic myringitis in two cases (1.24%). Anterior reperforation can be explained by the slipping of the cartilage making a gap between the graft and the remaining eardrum. Such failure is related to the surgical technique: when the closure of the anterior part of the tympanic perforation was not complete, that is why the surgeon should do his best, during myringoplasty, to control the anterior angle by reaming the external auditory canal or mobilizing the patient’s position. A good exposure offering a good control of all the compartments of the tympanic cavity is the best guarantee for a successful myringoplasty. Localization of the first tympanic perforation seems to be influencing anatomical results; it was noted that subtotal perforations were more likely to reperforate (12.2%).
Among the 9 cases of reperforations, 3 cases benefited from a surgical revision with placement of a perichondrium-reinforced in toto-cartilage graft with a good final result.
In our study, the different factors that could have influenced these results were identified (Table 1), and only a history of chronic rhinosinusitis was found to be significantly correlated with a higher anatomical failure rate with an estimated risk of 4.29. This may be explained by tubal dysfunction resulting in poor aeration of the middle ear and exposure of its mucosa to mediators of chronic inflammation.
The first audiometric control was performed between the third and sixth postoperative month. The average air conduction hearing threshold decreased from 36.1 dB preoperatively to 24.8 dB postoperatively: significant audiometric gain on all sound frequencies (Table 2).
The average preoperative Rinne was 26.20±7.05 dB. The average residual Rinne was 14.72±9.08 dB, that is an average gain of 11.48±8.62 dB. This hearing improvement was statistically significant (p<0.001). We obtained a good functional result (residual Rinne ≤20 dB) in 91.9% of cases and a closure of the Rinne (residual Rinne ≤10 dB) in 50.3% of cases.
After a univariate analytical study, the main factors that proved to have a significant influence on the functional result were: the site and the size of the perforation, the state of the mucous membrane of the tympanic cavity, the state of the ossicular chain (complete or lysed), the preoperative Rinne and the anatomical result. Age, gender, history of otologic surgery, etiology of tympanic perforation, status of the tympanic remnant, status of the contralateral ear, and graft material did not influence the functional outcome of myringoplasty. After a multivariate study, we retained only the anatomical result of the myringoplasty as a factor having a significant impact on the auditory result (Table 3).
A good anatomical result is significantly correlated with a good functional result (p=0.015). The average hearing gain is also better in case of anatomical success but the difference is not statistically significant (p=0.10).
Myringoplasty or tympanoplasty type 1 is an otologic surgery that aims to repair the loss of substance of a perforated tympanic membrane, in order to limit chronic inflammatory pathology of the middle ear and improve hearing. The use of cartilage as a tympanic membrane repair material has become commonly used by otologists [2]. A review of the literature [6] showed the superiority of cartilage compared to fascia temporalis due to its higher success rate and low incidence of reperforation. This type of graft feeds by diffusion from the surrounding tissue such as the perichondrium and tympanic-meatal flap and is easily integrated into the tympanic membrane due to its flexibility. Its rigid character makes it robust and resistant to resorption and retraction under prolonged pressure [7-10]. This resistance is more marked when the cartilage is grafted with its perichondrium [9,10]. This rigidity initially raised doubts about the auditory result [2,8], but several publications have had encouraging results [7,11,12].
Our study is interested in evaluating the use of cartilage (tragal or chonqual) as a material for repairing tympanic perforations resulting from simple chronic otitis media or in some cases from post-traumatic tympanic perforations.
Since its introduction, the use of cartilage has undergone several techniques. In our series, all cases were operated on by the underlay technique using in toto-cartilage, reinforced, in some cases, by perichondrium, with a notch to transpose the malleus handle.
The markers of a good anatomical result after myringoplasty were considered to be the complete and definitive closure of the tympanic perforation and the good condition and position of the neotympanum. The overall anatomical success rate in our series was estimated at 93.2%. In the literature, the anatomical success rate of myringoplasty varies between 90% and 96.1% [5,13,14]. In all studies, no cases of cartilage graft resorption or retraction were found, supporting the idea that cartilage is more resistant and superior to other types of grafts [13]. The cases of reperforations found in our study represent 5.6% of the total number of myringoplasties, that rate is comparable to the results reported in the literature. In other study, the reperforation rate was 4.8% [15]. Reperforations can occur early during the first three months after surgery. There were 1.8% cases of cartilage graft dehiscence (by slippage). It was reported that cartilage graft dehiscence rate is 2.2% [1]. It was found that the most common situations for reperforation were initial subtotal perforations (87.5%) and anterior perforations [16].
The hearing success rate (residual Rinne of ≤20 dB) in our study was 91.9%, a result close to those found in the literature (from 81.6% to 96%) [4,17]. These good functional results support the superiority of cartilage as the material of choice for tympanic membrane repair. In our study, we noted a very significant improvement in hearing threshold (p<0.001). The calculated average gain was 11.48 dB. This result is close to those found in other series [18-22]. The average residual Rinne found in our study was 14.72 dB. This result is also comparable to those found in the literature [3,20,21,23]. These results further dissipate the doubts initially raised about a possible negative impact of cartilage on hearing.
The recent bibliography specifies the interest of the new endoscopic approach, particularly in the repair of large perforations; transcanal endoscopic myringoplasty for large tympanic membrane perforations using a double-layer perichondrium and cartilage graft is feasible with comparable rates of closure to more invasive approaches [24]. And new other therapeutic methods have been published with the aim to improve therapeutic results in the repair of eardrum perforations such as the use of cartilage-perichondrium double graft combined with basic fibroblast growth factor, which has been demonstrated as effective method for providing the long-term graft success rate of the perforations with extensive epithelialization [25].
Several factors can influence the anatomical and functional results of myringoplasty. According to the literature, certain factors have been correlated with a high failure rate, hence the term “high-risk ears.” Several studies [21,23] have demonstrated a significant relationship between the presence of chronic rhinosinusitis pathologies and anatomical failure. In our study, the presence of such a history multiplied the risk of failure by 4.29 (OR=4.29). This encouraged us to restore tubal function before any myringoplasty. Concerning the functional result, we have retained only the anatomical result of myringoplasty as a factor significantly influencing the functional result.
Acknowledgments
All my thanks to the instrumentalists of the operating room and to the technicians working in the audiometry unit, at at the University Hospital “Fattouma Bourguiba” Monastir-Tunisia.
Notes
Author Contributions
Conceptualization: Naourez Kolsi. Data curation: Naourez Kolsi, Mahdi Ferjaoui, Rachida Bouatay. Formal analysis: Naourez Kolsi. Methodology: Naourez Kolsi, Nawress Bouaziz. Software: Naourez Kolsi. Supervision: Khaled Harrathi, Jamel Koubaa. Validation: Naourez Kolsi. Visualization: Naourez Kolsi. Writing—original draft: Naourez Kolsi, Nawress Bouaziz. Writing—review & editing: Naourez Kolsi. Approval of final manuscript: all authors.
Fig. 1.
Retro-auricular surgical approach. A: Incision of the posterior wall of the external auditory canal. B: Detachment of the tympanomeatal flap. C: Detachment of the malleus handle and preparation for placement of the graft.
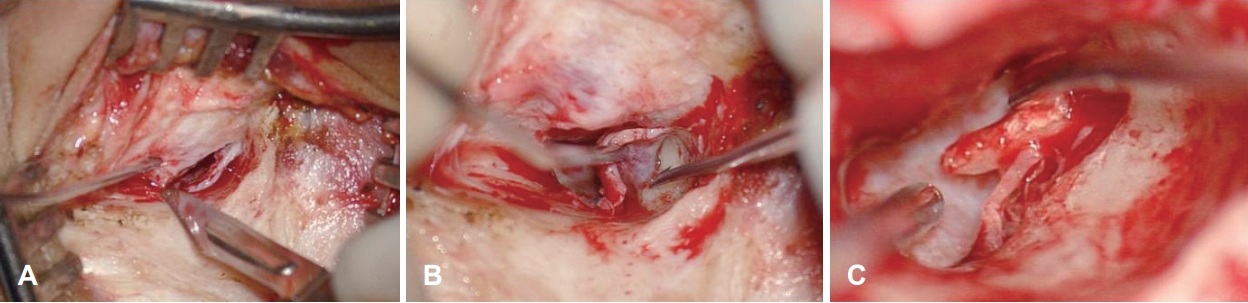
Fig. 2.
Removal and preparation of the cartilage graft. A: Cartilage sample from the tragus. B: Detachment of its perichondrium on one of its facets. C: Making a notch in the cartilage graft that will hug the handle of the malleus.
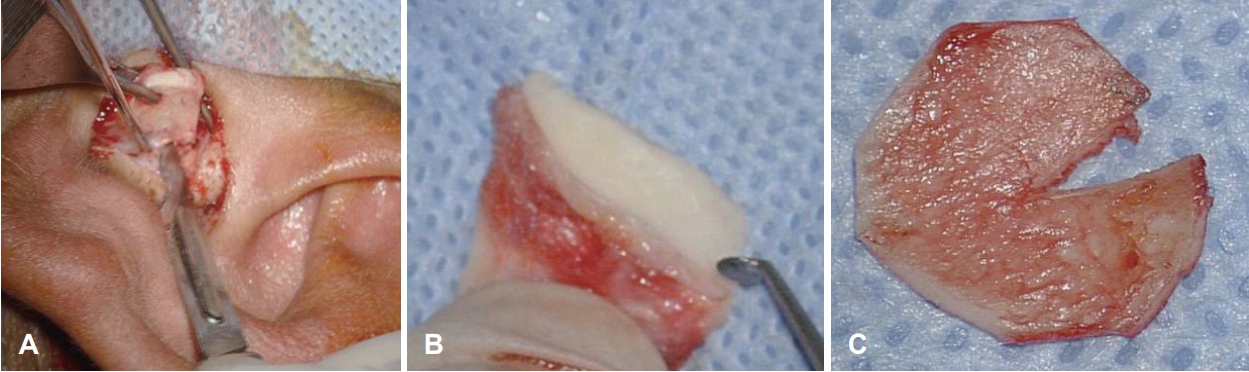
Fig. 3.
Otoendoscopic view after surgical repair of the tympanic perforation using cartilage from tragus (right ear).
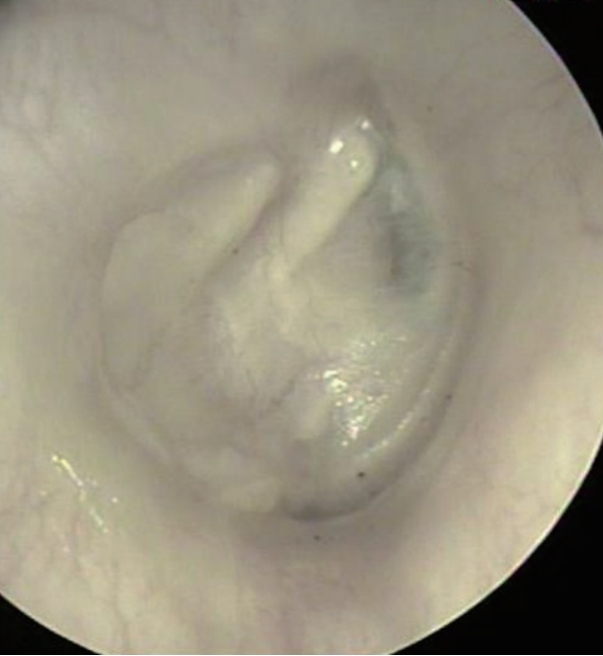
Table 1.
Summary of factors influencing the anatomical result after cartilage myringoplasty
| Study factors | Success rate (%) | Failure rate (%) | OR | p |
|---|---|---|---|---|
| History of otologic surgery | 0.57 | |||
| Yes | 95.8 | 4.2 | ||
| No | 92.7 | 7.3 | ||
| History of chronic rhinosinusitis | 4.29 | 0.009* | ||
| Yes | 78.9 | 21.1 | ||
| No | 95.1 | 4.9 | ||
| Ear drying time | 0.26 | |||
| <3 months | 88.0 | 12.0 | ||
| ≥3 months | 94.1 | 5.9 | ||
| Perforation site | 0.19 | |||
| Anterior | 93.8 | 6.2 | ||
| Subtotal | 88.8 | 11.2 | ||
| Inferior | 100.0 | 0.0 | ||
| Central | 100.0 | 0.0 | ||
| Tympanic residue | 0.10 | |||
| Normal | 91.6 | 8.4 | ||
| Calcareous deposit | 100.0 | 0.0 | ||
| Controlateral tympan | ||||
| Normal | 92.0 | 8.0 | 0.54 | |
| Pathologic | 94.5 | 5.5 | ||
| Tympanic cavity mucosa | 0.45 | |||
| Healthy | 96.4 | 3.6 | ||
| Pathologic | 92.5 | 7.5 | ||
| Cartilage | 0.29 | |||
| Tragal | 95.6 | 4.4 | ||
| Conqual | 91.4 | 8.6 | ||
| Graft | 0.24 | |||
| Cartilage+perichondrium | 96.4 | 3.6 | ||
| Cartilage only | 91.7 | 8.3 |
Table 2.
Average auditory thresholds in air conduction (AC) before and after surgery
| Auditory frequencies |
Auditory thresholds in AC (dB) |
p | |
|---|---|---|---|
| Preoperativerly | Postoperatively | ||
| 500 Hz | 45.3 | 26.8 | <0.001 |
| 1,000 Hz | 37.8 | 24.6 | |
| 2,000 Hz | 25.2 | 23.0 | |
| Average | 36.1 | 24.8 | |
Table 3.
Factors influencing functional outcome in multivariate analysis
| Study factors | B | SD | 95% CI | p |
|---|---|---|---|---|
| Perforation site | 0.543 | 0.505 | 0.639-4.633 | 0.283 |
| Perforation size | -0.726 | 1.235 | 0.043-5.451 | 0.557 |
| Rinne >30 dB | 0.526 | 0.694 | 0.434-6.60 | 0.448 |
| Complete ossicular chain | -1.228 | 0.801 | 0.061-1.407 | 0.125 |
| Condition of the mucous membrane of the tympanic cavity | -0.249 | 0.747 | 0.172-3.224 | 0.649 |
| Anatomical result | -1.296 | 0.948 | 0.023-0.934 | 0.042* |
REFERENCES
1. Gamra OB, Mbarek C, Khammassi K, Methlouthi N, Ouni H, Hariga I, et al. Cartilage graft in type I tympanoplasty: audiological and otological outcome. Eur Arch Otorhinolaryngol 2008;265:739–42.



3. Dornhoffer J. Cartilage tympanoplasty: indications, techniques, and outcomes in a 1,000-patient series. Laryngoscope 2003;113:1844–56.


4. Demirpehlivan IA, Onal K, Arslanoglu S, Songu M, Ciger E, Can N. Comparison of different tympanic membrane reconstruction techniques in type I tympanoplasty. Eur Arch Otorhinolaryngol 2011;268:471–4.



5. Chen XW, Yang H, Gao RZ, Yu R, Gao ZQ. Perichondrium/cartilage composite graft for repairing large tympanic membrane perforations and hearing improvement. Chin Med J (Engl) 2010;123:301–4.

6. Iacovou E, Vlastarakos PV, Papacharalampous G, Kyrodimos E, Nikolopoulos TP. Is cartilage better than temporalis muscle fascia in type I tympanoplasty? Implications for current surgical practice. Eur Arch Otorhinolaryngol 2013;270:2803–13.



7. Hasaballah MS, Hamid OAMA, Hamdy TAH. Audiological and otological outcome in Bi-island chondroperichondrial graft type I tympanoplasty. Egypt J Ear Nose Throat Allied Sci 2014;15:183–8.

8. Lyons SA, Su T, Vissers LE, Peters JP, Smit AL, Grolman W. Fascia compared to one-piece composite cartilage-perichondrium grafting for tympanoplasty. Laryngoscope 2016;126:1662–70.



9. Yamamoto E, Iwanaga M, Fukumoto M. Histologic study of homograft cartilages implanted in the middle ear. Otolaryngol Head Neck Surg 1988;98:546–51.



10. Elwany S. Histochemical study of cartilage autografts in tympanoplasty. J Laryngol Otol 1985;99:637–42.


12. Cavaliere M, Mottola G, Rondinelli M, Iemma M. Tragal cartilage in tympanoplasty: anatomic and functional results in 306 cases. Acta Otorhinolaryngol Ital 2009;29:27–32.


13. Vashishth A, Mathur NN, Choudhary SR, Bhardwaj A. Clinical advantages of cartilage palisades over temporalis fascia in type I tympanoplasty. Auris Nasus Larynx 2011;41:422–7.


14. Kaya I, Benzer M, Uslu M, Bilgen C, Kirazli T. Butterfly cartilage tympanoplasty long-term results: excellent treatment method in small and medium sized perforations. Clin Exp Otorhinolaryngol 2018;11:23–9.




15. Callioglu EE, Ceylan BT, Kuran G, Demirci S, Tulaci KG, Caylan R. Cartilage graft or fascia in tympanoplasty in patients with low middle ear risk index (anatomical and audological results). Eur Arch Otorhinolaryngol 2013;270:2833–7.



16. Altuna X, Navarro JJ, Martínez Z, Lobato R, Algaba J. Island cartilage myringoplasty. Anatomical and functional results in 122 cases. Acta Otorrinolaringol Esp 2010;61:100–5.


17. Pfammatter A, Novoa E, Linder T. Can myringoplasty close the airbone gap? Otol Neurotol 2013;34:705–10.


18. Balaguer García R, Morales Suárez-Varela MM, Tamarit Conejeros JM, Agostini Porras G, Murcia Puchades V, Dalmau Galofre J. Myringoplasties. A retrospective analysis of our surgical outcomes. Acta Otorrinolaringol Esp 2011;62:213–9.


19. De Seta E, De Seta D, Covelli E, Viccaro M, Filipo R. Type I tympanoplasty with island chondro-perichondral tragal graft: the preferred technique? J Laryngol Otol 2013;127:354–8.


20. Michel G, Espitalier F, Boyer J, Malard O, Bordure P. Clinical and economic evaluation of minimally invasive cartilaginous palisade myringoplasty. Acta Otolaryngol 2018;138:10–5.


21. Yilmaz MS, Kara A, Guven M, Demir D, Erkorkmaz U. Assessment of the factors that affect the anatomic and functional success of cartilage tympanoplasty in children. J Craniofac Surg 2017;28:e106–10.


22. Dinc ASK, Cayonu M, Boynuegri S, Sahin MM, Paksoy B, Eryilmaz A. Graft success and hearing results between cartilage island graft and temporal muscle fascia graft myringoplasty. J Coll Physicians Surg Pak 2020;30:33–6.


23. Callioglu EE, Bercin AS, Kale H, Muderris T, Demirci S, Tuzuner A, et al. Is allergic rhinitis a factor that affects success of tympanoplasty? Acta Medica (Hradec Kralove) 2016;59:10–3.