Introduction
Lyme disease is a bacterial infection typically transmitted to humans through the bite of an infected tick. It is caused by the bacterium
Borrelia burgdorferi and can affect multiple organs and systems in the body [
1]. One of the less common but potentially serious complications of Lyme disease is neurosensory hearing loss, which can occur when the infection spreads to the nerves and tissues in the ear [
2].
Previous literature extensively studied the potential impact of Lyme disease on the auditory system, particularly neurosensory hearing loss [
3,
4]. Some studies reported cases of Lyme disease presenting with sudden onset or progressive hearing loss as the primary or sole symptom. These cases emphasize the importance of considering Lyme disease as a potential cause when evaluating patients with unexplained hearing loss [
1].
The exact mechanism by which Lyme disease leads to neurosensory hearing loss is not fully understood, but it is believed to be related to the inflammatory response triggered by the infection [
5]. Inflammation plays a significant role in the pathogenesis of hearing loss in Lyme disease. The immune response aimed at combating the
B. burgdorferi bacteria can lead to the release of inflammatory mediators, which may damage the delicate structures of the inner ear, including the cochlea and associated nerves. This inflammatory damage disrupts the normal transmission of sound signals, resulting in hearing loss [
6].
Given the non-specific nature of Lyme disease symptoms and the potential delay in their onset, diagnosing Lyme-related neurosensory hearing loss can be challenging. Timely recognition and treatment of Lyme disease are essential to prevent complications, including hearing loss [
3-
5,
7]. Healthcare professionals should maintain a high index of suspicion for Lyme disease, especially in patients living in or visiting endemic areas, who present with sudden or unexplained hearing loss [
7].
This case highlights the need for increased awareness of Lyme disease as a potential cause of sudden-onset neurosensory hearing loss. A comprehensive understanding of the relationship between Lyme disease and hearing loss will help healthcare providers make accurate diagnoses and initiate appropriate treatment strategies promptly.
Case Report
A 23-year-old woman with no prior medical history visited the outpatient clinic of our hospitalŌĆÖs ENT department with a 2-month history of temporal headache, tinnitus, and instability. This was followed by a sudden bilateral hearing loss, with no accompanying symptoms such as fever, otorrhea, rotatory vertigo, facial palsy, or cutaneous rash.
Upon examination, the patientŌĆÖs right and left auricles and external auditory canals were normal, and both tympanic membranes appeared normal as well. There was no spontaneous nystagmus or ataxia observed. The sinusoidal gaze tracking was normal, and the Romberg test yielded normal results. However, the head-thrust test performed to the left was positive. Additionally, the Fukuda step test was positive, with the patient rotated to the left. The remainder of the examination, including skin, joint, and neurologic assessments, was normal.
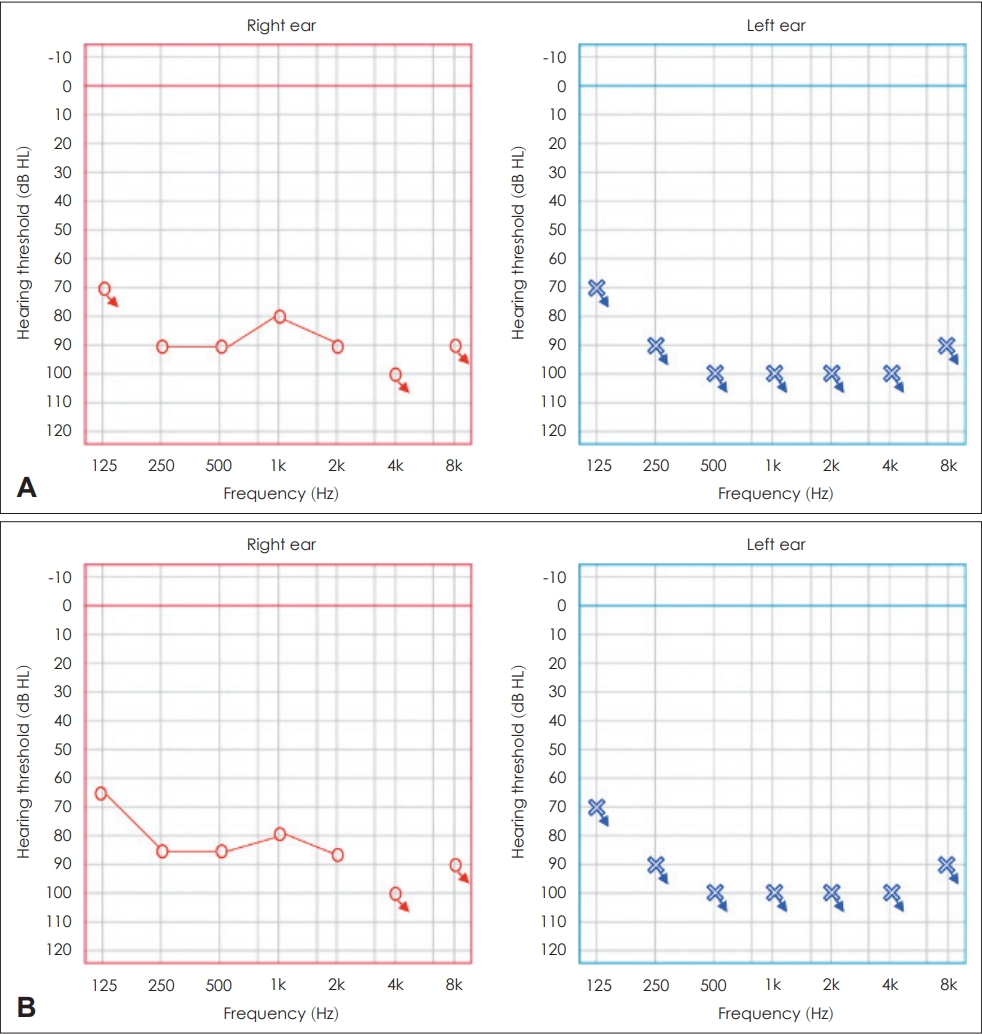
Pure-tone audiometry test revealed complete perceptive hearing loss in the left ear with thresholds of over 100 dB and profound hearing loss in the right ear with average thresholds of 90 dB (
Fig. 1A).
A videonystagmography was conducted and revealed a compensated hyporeflexia of the left canal at 47.9% on very low frequencies. However, the rest of the examination, which included tests for slow pursuit, saccade, and optokinetic reflex, was normal.
An MRI revealed an intrasellar arachnoidocele with dilation of the optic nerve sheaths, but ophthalmologic examination showed no abnormalities.
In accordance with SHL guidelines, corticotherapy was initiated following StennertŌĆÖs protocol.
Additional tests were conducted and revealed that the patientŌĆÖs complete blood count with differential count was normal. Serological tests for syphilis, HIV, toxoplasmosis, rubella,
Cytomegalovirus, HSV-1, HSV-2, and mumps virus were negative. Blood tests for
B. burgdorferi antibodies showed positive results for IgM and negative results for IgG, which were confirmed by a Western blot test 10 days later. The patient was prescribed a 21-day course of doxycycline at 100 mg twice daily for the treatment of neuroborreliosis. A follow-up blood test conducted 4 days after the start of antibiotics showed IgM traces but no IgG. However, despite treatment, the patient did not experience any improvement in her hearing loss (
Fig. 1B). As a result, she is now being considered for a cochlear implant.
Discussion
There is still a lack of full understanding regarding the causes of sudden sensorineural hearing loss (SHL). However, some potential etiological factors behind the disease have been proposed, including autoimmune diseases, viral or bacterial infections, and vascular insults [
8].
Lyme disease is known to be one of the causative agents of sudden SHL. The disease is a multi-system illness caused by the tick-borne
B. burgdorferi and can cause varying symptoms in different stages, primarily affecting the skin, nervous system, heart, and joints. In the later stages of Lyme disease, neuroborreliosis can occur. This can result in associated symptoms such as headache, fatigue, arthritic fever, and malaise, with head and neck involvement commonly observed in many patients [
1,
7].
It is thought that the bacteria may cause an inflammatory response in the tissues of the inner ear, leading to damage to the hair cells or nerve fibers responsible for hearing. Additionally, the bacteria may directly invade and damage these structures. It is also possible that the hearing loss is a result of the bodyŌĆÖs immune response to the bacteria, which can cause damage to healthy tissues as well [
1]. An apoptotic reaction in the cochlea may be triggered by
Borrelia infection, even in the absence of disseminated neuroborreliosis and central nervous system antibodies [
9].
According to a systematic literature search conducted in 2013 by Peeters, et al. [
7], the prevalence of Lyme disease in patients with sudden deafness ranges between 0% and 21.3%. The actual percentage appears to be dependent on the concentration of infected ticks in a given country or locality, as well as the diagnostic tests used to confirm Lyme disease [
7].
The absence of a tick bite or skin rash in cases of
Borrelia infection can make it difficult to suspect the diagnosis based solely on clinical history, since ticks are small and a rash may not always appear [
10].
In our case, despite conducting all the standard paraclinical examinations as per the guidelines, there was no clear etiology identified for the SHL. Therefore, we conducted a Lyme IgG and IgM test on the serum, which turned out to be positive for IgG. We then proceeded to perform a Western blot on the cerebrospinal fluid to confirm the possibility of Lyme disease as a potential cause.
Authors are currently engaged in significant debate on whether the diagnosis of neuroborreliosis should be considered and whether a biological diagnosis should be routinely conducted when a patient presents with a sudden onset of SHL.
Given the significance of early diagnosis in this pathology and its potential to cause damaging complications, some authors recommend that biological testingŌĆöserology for Lyme disease in both plasma (Lyme IgG and IgM) and cerebrospinal fluid (western blot)ŌĆöshould be systematically performed in etiological tests for patients with SHL [
8,
11,
12].
Conversely, Peeters, et al. [
7], Saunders [
9], van der Heijden, et al. [
13], and Peltomaa, et al. [
2] concur that clinicians should rely on their diagnostic expertise to identify which patients are at risk of this specific etiology (among others). They also emphasize the significance of screening based primarily on the patientŌĆÖs history of erythema migrans, combined with fever and headache.
Initially, our patient was treated with corticosteroids following StennertŌĆÖs protocol for sudden SHL, prior to the confirmation of the Lyme disease diagnosis. Subsequently, the patient was prescribed doxycycline for neuroborreliosis and tested positive for Lyme IgM with no presence of IgG in the biological control. Unfortunately, the patientŌĆÖs hearing loss did not recover.
Two case reports [
12,
14] and one patient in the study conducted by Hanner, et al. [
15] were the only instances of reported recovery of hearing loss in patients with confirmed Lyme disease and sudden deafness, according to a literature review [
7].
In conclusion, our case highlights the occurrence of bilateral SHL in Lyme disease, with recovery being reported in some cases after treatment but with persistence of hearing loss also a significant possibility.
We recommend testing for Lyme disease in cases of bilateral SHL, particularly in patients with a history of tick bites or in endemic areas, and even when no clinical history is present and paraclinical examinations are inconclusive. Early diagnosis is crucial in preventing serious and irreversible complications.