|
 |
- Search
| J Audiol Otol > Volume 17(1); 2013 > Article |
Abstract
Salicylate, the active ingredient of aspirin can cause sensorineural hearing loss and tinnitus when plasma concentrations reach a critical level. The ototoxic mechanisms of salicylate remain unclear but hearing and tinnitus usually recovers a few days after intoxication. There have been few reports of salicylate-induced ototoxicity in Korea, and the majority is caused by a low dose of aspirin. Herein, we report a case of sudden hearing loss and tinnitus after acute salicylate intoxication and review recent updates on salicylate ototoxicity.
Aspirin is one of the most popular drugs used for pain relief, antipyretic, antithrombotic and anti-inflammatory purposes. However, several side effects have been reported, including gastric eruption, and renal and hepatic dysfunction, following chronic therapeutic dosage. Acute salicylate intoxication is a serious condition that can be fatal. Reversible hearing loss and tinnitus are well-known side effects of salicylate toxicity but the mechanism has not been revealed.1) We experienced a case of sudden bilateral sensorineural hearing loss due to acute salicylate intoxication and present the clinical course and characteristics in this report.
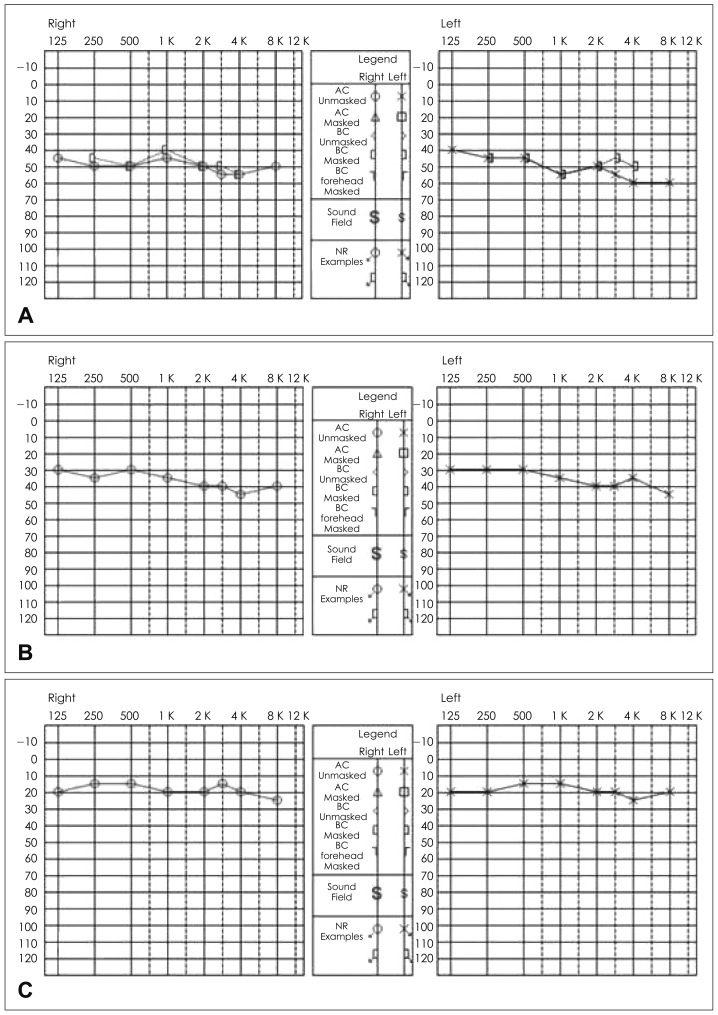
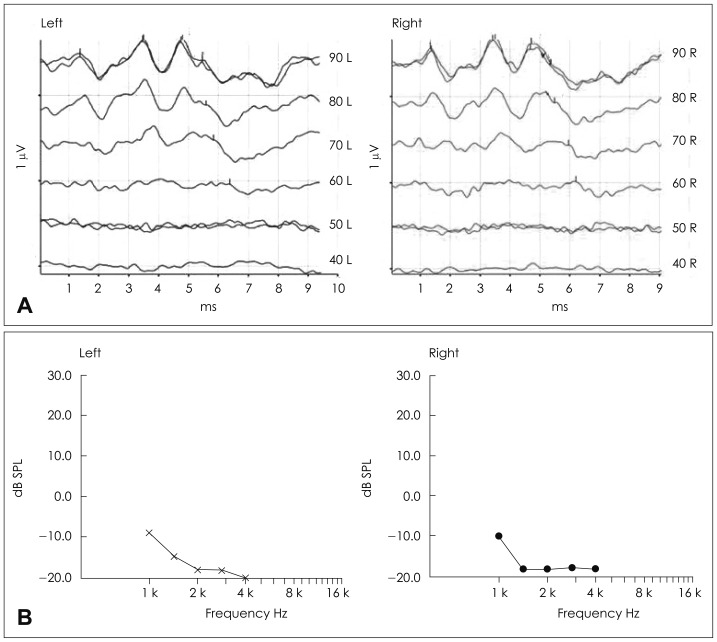
A 46-year-old female (42 kg) was taken to the emergency unit with her husband. Her mental status was drowsy and she was reported to have taken 200 tablets of aspirin (325 mg├Ś200 tablets=65000 mg) with an alcoholic beverage (soju, alcohol content 19%, 200 mL). A blood sample was taken immediately and showed no abnormality of liver or renal function. The electrolyte profile was also within normal values but arterial blood gas analysis showed metabolic acidosis (pH 7.39, pCO2 33 mm Hg, and bicarbonate 21.7 mmEq/L). Urine chemistry was normal. A nasogastric tube was inserted and activated charcoal and intravenous fluids administered to remove the remaining salicylate in her body. Sodium bicarbonate was used for the correction of metabolic acidosis. She found that her hearing deteriorated and tinnitus developed on the second hospital day, and she was subsequently referred to our department. She was stable in terms of mental status, and her metabolic acidosis was corrected at the time of otologic assessment. Both middle ears were clear in otoscopic views. Neurological examination also revealed no abnormal findings. Pure tone audiometry (PTA) showed bilateral symmetric sensorineural hearing loss with a threshold of 50 dB HL in all frequencies, and tinnitus was equivalent to the narrow-band noise of 4 kHz and 5-10 dB SL bilaterally (Fig. 1A). A high-dose oral steroid (prednisolone 60 mg/day) regimen was initiated following medical consultation. Hearing thresholds were unchanged on follow-up PTA and were 60 dB nHL by auditory brainstem response (Fig. 2A). Distortion product otoacoustic emission showed no response on both ears (Fig. 2B). On the fourth hospital day, PTA thresholds improved to the level of 36 dB HL on both ears (Fig. 1B) but she refused further admission therapy. She received a daily dose of 60-mg oral prednisolone during the 4 days of admission, which was tapered as scheduled. She revisited the clinic 3 days later and PTA thresholds were normalized to 18 dB HL (Fig. 1C). However, she complained that her hearing had not fully recovered and tinnitus remained in the right ear. The tinnitus was equivalent to a pure tone of 125 Hz and 5-10 dB SL in the right ear. Monthly follow-up was scheduled without further medication; she last visited the clinic 4 months after intoxication. PTA thresholds were unchanged and she did not complain of hearing loss or tinnitus.
Salicylate ototoxicity can cause various degrees of hearing loss and tinnitus. Bilateral symmetric sensorineural hearing loss with a threshold range of 20-40 dB in all tested frequencies represents the characteristic audiologic results.2,3) Tinnitus and hearing loss are known to be reversible and recover several days after aspirin discontinuation.
There has been controversy regarding the mechanism of salicylate ototoxicity; many hypotheses have been proposed. Cochlear outer hair cells are the most widely accepted site of injury.4,5) Spiral ganglion cells represent another site of inflammation.6,7) Hypoxia caused by decreased blood flow to the cochlea has also been proposed as a mechanism of injury.8) On the contrary, chronic high-dose aspirin intake rather than acute intoxication can improve outer hair cell active movement. However, permanent hearing loss can occur despite the initial hearing improvement upon chronic high dose aspirin administration.9)
Tinnitus is the most constant and initial symptom of salicylate ototoxicity and is known to be reversible. It typically presents as a roaring hissing noise and matches high-pitched sounds.1) This was thought to be related to the increase in spontaneous activity of auditory nerves at any level in the auditory pathway.10,11) Myers and Bernstein2) found that the loudness of tinnitus had linear correlation with the salicylate blood concentration. Tinnitus developed at plasma levels below 100 mg/L and the loudness was equivalent to 60 dB at around 300 mg/L. Mongan, et al.12) proposed that a 300 mg/L plasma level of aspirin could be an index of the maximal therapeutic dosage. These reports suggest that the therapeutic dosage of aspirin should be adjusted individually based on monitoring of plasma salicylate levels.
The degree of hearing loss is also known to be proportional to the plasma concentration of salicylate.1,13) Day, et al.13) conducted clinical studies and found no ototoxicity in anti-platelet doses (<10 mg/L) of aspirin. However, hearing loss and tinnitus intensity increased progressively with plasma salicylate concentration from antipyretic (30-100 mg/L) to anti-inflammatory (150-300 mg/L) dosages. Myers and Bernstein2) reported that, as the plasma salicylate level approached 300 mg/L, a hearing loss of 30-40 dB occurred, but there was no correlation above 400 mg/L.
Although the estimated salicylate plasma concentration was higher in our case, the actual levels at which bilateral sudden hearing loss occurred were not revealed. When considering the individual variations of plasma concentration from the same dosage of aspirin12) and the loss of dose by gastric lavage, failure to monitor plasma salicylate concentration was a limitation of this study. However, according to the hearing thresholds and tinnitus intensity of the patient, the plasma salicylate concentration would be expected to exceed 300 mg/L.1,13)
The patient presented no abnormalities other than moderate bilateral sudden hearing loss with tinnitus and metabolic acidosis. Her hearing gradually improved from the fourth day of intoxication and normalized within 1 week. We prescribed high-dose steroids based on previous reports, though their effectiveness is controversial. One animal study concluded that premedication of steroids can reduce salicylate ototoxicty.14) Other cli-nical case report of low-dose aspirin ototoxicity treated with steroids showed their efficacy in aspirin-induced sudden hearing loss.15) However, high-dose steroid use is not recommended in cases of hearing loss during aspirin overdose, as it can lead to gastric complications such as bleeding.
Nausea, vomiting, diaphoresis, and tinnitus are the earliest signs and symptoms of general salicylate toxicity. Other early symptoms and signs are vertigo, hyperventilation, tachycardia, and hyperactivity. As toxicity progresses, agitation, delirium, hallucinations, convulsions, lethargy, and stupor may occur. Hyperthermia is an indication of severe toxicity, especially in young children. When aspirin toxicity is suspected, blood samples should be taken for analysis of serum glucose levels, electrolytes, and blood gas profiles. Initial treatment of an acute overdose involves resuscitation followed by gastric decontamination by administration of activated charcoal, which adsorbs the aspirin in the gastrointestinal tract. Urine alkalization and sufficient intravenous fluid administration are also required and hemodialysis is prepared for possible acute renal failure.
In summary, aspirin is an easily accessible anti-inflammatory drug, overdosing of which can cause reversible hearing loss and tinnitus. Physicians should be aware of this when they encounter aspirin ototoxicity in patients.
References
1. Cazals Y. Auditory sensori-neural alterations induced by salicylate. Prog Neurobiol 2000;62:583ŌĆō631. PMID: 10880852.


2. Myers EN, Bernstein JM. Salicylate ototoxicity; a clinical and experimental study. Arch Otolaryngol 1965;82:483ŌĆō493. PMID: 4954319.


3. Lee HY, Yeo SW, Chae SY, Choi YC, Park YS, Kim J. A morphological study on the cochlea in the rats of Na-salicylate induced ototoxicity. Korean J Audiol 1998;2:124ŌĆō129.
4. Kakehata S, Santos-Sacchi J. Effects of salicylate and lanthanides on outer hair cell motility and associated gating charge. J Neurosci 1996;16:4881ŌĆō4889. PMID: 8756420.


5. Lue AJ, Brownell WE. Salicylate induced changes in outer hair cell lateral wall stiffness. Hear Res 1999;135:163ŌĆō168. PMID: 10491964.


6. Feng H, Yin SH, Tang AZ, Tan SH. Salicylate initiates apoptosis in the spiral ganglion neuron of guinea pig cochlea by activating caspase-3. Neurochem Res 2011;36:1108ŌĆō1115. PMID: 21451968.


7. Wei L, Ding D, Salvi R. Salicylate-induced degeneration of cochlea spiral ganglion neurons-apoptosis signaling. Neuroscience 2010;168:288ŌĆō299. PMID: 20298761.



8. Cazals Y, Li XQ, Aurousseau C, Didier A. Acute effects of noradrenalin related vasoactive agents on the ototoxicity of aspirin: an experimental study in the guinea pig. Hear Res 1988;36:89ŌĆō96. PMID: 3143707.


9. Chen GD, Kermany MH, D'Elia A, Ralli M, Tanaka C, Bielefeld EC, et al. Too much of a good thing: long-term treatment with salicylate strengthens outer hair cell function but impairs auditory neural activity. Hear Res 2010;265:63ŌĆō69. PMID: 20214971.



10. Basta D, Ernst A. Effects of salicylate on spontaneous activity in inferior colliculus brain slices. Neurosci Res 2004;50:237ŌĆō243. PMID: 15380332.


11. Ochi K, Eggermont JJ. Effects of salicylate on neural activity in cat primary auditory cortex. Hear Res 1996;95:63ŌĆō76. PMID: 8793509.


12. Mongan E, Kelly P, Nies K, Porter WW, Paulus HE. Tinnitus as an indication of therapeutic serum salicylate levels. JAMA 1973;226:142ŌĆō145. PMID: 4740906.


13. Day RO, Graham GG, Bieri D, Brown M, Cairns D, Harris G, et al. Concentration-response relationships for salicylate-induced ototoxicity in normal volunteers. Br J Clin Pharmacol 1989;28:695ŌĆō702. PMID: 2611090.



14. Jang WI, Kim YS, Kim DW, Lee BD. A case of bilateral sudden sensorineural hearing loss occurring after taking the aspirin. J Clin Otolaryngol Head Neck Surg 2010;21:67ŌĆō70.

15. Nam BH, Kim PS, Park YS, Worrell LA, Park SK, John EO, et al. Effect of corticosteroid on salicylate-induced morphological changes of isolated cochlear outer hair cells. Ann Otol Rhinol Laryngol 2004;113:734ŌĆō737. PMID: 15453532.